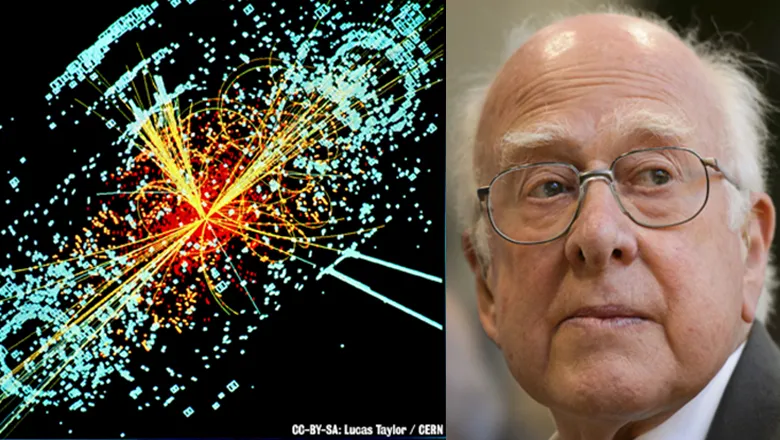
Remembering Professor Peter Higgs (1929 – 2024)
King’s alumnus and Nobel Prize winner Professor Peter Higgs has passed away aged 94
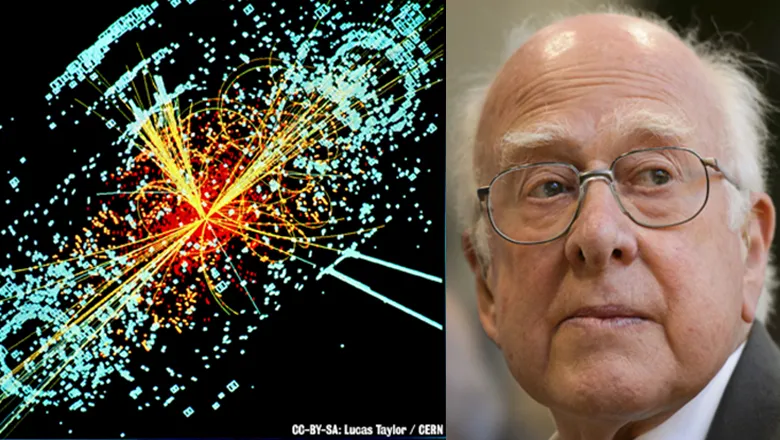
King’s alumnus and Nobel Prize winner Professor Peter Higgs has passed away aged 94

Attempts by the WHO to push for an agreement in the Pandemic Treaty negotiations are detrimental to poorer countries, according...

The team received awards for reducing food waste, promoting sustainability and providing nutritious food

The Faculty of Dentistry, Oral & Craniofacial Sciences held their first ever Staff Awards on Thursday 18 April.

A recent public engagement project carried out across King’s College London, University College London, and Queen Mary...

A new podcast episode explores how the far-right has seen its popularity grow across Europe in recent years and how this is...


An evidence-based intervention to support personal recovery developed by researchers at King’s is improving patient experience...

Forced displacement is a growing problem around the world. In 2015 the United Nations reported that 60 million people worldwide...

Historically menopause has been overlooked and trivialised. Though a natural process, for some women physical and psychological...

Cigarettes kill over half of their long-term users. The World Health Organisation (WHO) considers the tobacco epidemic to be one...

Why is that India's voters appear to place curiously little emphasis on health when it comes to voting decisions? Professor...

The origin, or 'provenance' of data is important to gaining trust in policies and processes that are data driven.
Providing information and resources for journalists and media professionals.