It’s a very new direction for our lab to do this type of big data bio-informatics analysis, when you take individual cells and literally probe them for every single gene and it’s really brought home to me just how powerful this approach is.
Dr Matthew Grubb, Grubb lab leader, Institute of Psychiatry, Psychology & Neuroscience, King's College London
24 July 2020
King's neuroscientists collaborate to work out the COVID-19 smell conundrum
A team of neuroscientists from King’s College London have collaborated with researchers from leading US universities on a project investigating the possible cellular and genetic mechanisms behind the loss of smell in COVID-19 patients.
The first results from the collaboration have now been published in the journal Science Advances.
Nearly 60% of people testing positive for COVID-19 suffer from a loss of smell or taste according to the COVID symptom tracker app developed by King’s College London and Zoe, and a loss of changed sense of smell and taste has now been added to the NHS COVID-19 symptom list. As a result, many questions are being asked about this symptom and how important it is to understanding the SARS CoV-2 virus.
Collaboration on anosmia

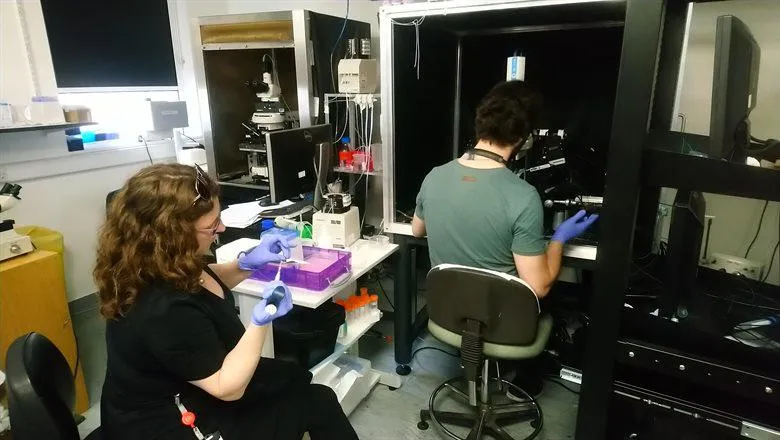
Usually the lab led by Dr Matthew Grubb study the system involved in our sense of smell (the olfactory system) as means to investigate how neurons change, develop and regenerate in the brain. After seeing a tweet about a preprint on the fundamental science behind COVID-19-related anosmia or loss of smell, the team are now involved in an exciting collaboration with Harvard University, University of California and Duke University amongst others. The piece of the jigsaw that the King’s lab is providing, spearheaded by senior post-doc Dr Marcela Lipovsek, is an analysis into which cells in the brain might or might not be involved in anosmia in COVID-19.
‘I’ve never done anything remotely disease related before,’ says Dr Grubb about his contribution to the research. ‘As a basic neuroscientist you always dream that maybe you’ve found something that might be useful in the medical world … so perhaps this is a start in that direction.’
New directions
The Grubb lab at the Institute of Psychiatry, Psychology & Neuroscience (IoPPN) are usually interested in the olfactory system because it’s a great model for asking how cells change and adapt to different sensory environments. As such they have access to huge genetic datasets on some of the neurons involved in smell.
He continued, ‘We already had the data but we had been analysing it for a completely different reason. In transcriptomics you have all the information about every gene whether you’re interested in it or not, which meant we could very easily look at the genetic data for thousands of cells to see if they might be involved in anosmia and COVID-19. It all happened amazingly quickly and was very different to how we normally do science.’
Video source: HORIZON – The EU Research & Innovation magazine
Loss of smell
Loss of smell usually happens for one of three reasons: the nose is blocked, the neurons in the brain or nose involved in smell are damaged, or the cells that support these sensory neurons are damaged which means the neurons can no longer function properly. The research suggests that the latter is the most likely explanation.
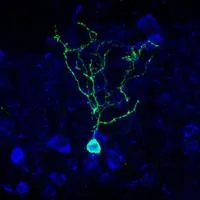
The molecular route that SARS-CoV-2 takes to infect cells uses two proteins: ACE2 acts as a receptor so the virus can attach to the surface of the cell, and TMPRSS2 allows the virus’ membrane to fuse with the membrane of the human cell. The new study involving the King’s College London research team analysed the genetic signs that these two phases of the infection could happen in the olfactory system. They examined which cells are showing the genetic activity needed to produce the two proteins ACE2 and TMPRSS2 by ascertaining the presence of the proteins’ mRNA, which is one of the essential stepping stones from gene to gene expression.
The research teams from the US showed that in the nose the sensory neurons for smell don’t have the mRNA needed for production of ACE2 and TMPRSS2. Alongside this the analysis by Dr Grubb’s team also showed that the neurones in the first part of the brain to process smell information – the olfactory bulb – do not have the required mRNA for these two proteins either.
Supporting cells
Taken together the results indicate that neither the neurons in the nose nor the brain are at the heart of anosmia in COVID-19 patients. This suggests that the loss of smell during COVID-19 infection is unlikely to be down to a direct infection of the brain cells. The study did show that a type of cell in the nose called the sustentacular cell shows mRNA for both the proteins. This type of cell physically and metabolically supports the neurons in the nose involved in smell. Whilst in the brain, there are low levels of ACE2 in cells called pericytes which are cells found in the lining of capillaries.
It may be that the infection of sustentacular cells and potentially the pericyte cells by SARS Cov-2 could make it difficult for the neurons involved in smell to function properly.
What we can say from our research is which cells are likely to be susceptible to the virus which is very revealing because of the clarity of the results.
Dr Matthew Grubb, Grubb lab leader, IoPPN
He added, ‘In the early days of the disease there were concerns that the virus might be neuroinvasive but, as far as we can tell, if the virus is affecting the olfactory bulb then it probably isn’t doing it via the neurons but via some other type of cells.’
Dr Grubb does stress that the data on the brain used in the study were from animals but he also highlights the olfactory system is very similar in humans. The research does not give insight into the nature of the damage done to cells but the data from the nose and the brain show very similar results in terms of indicating which cells are and aren’t involved in anosmia.
‘One thing that staggered me was just how coherent it all is,’ remarked Dr Grubb. ‘Normally you bring four or five research groups together and they can’t agree on much but for this everyone’s data and analysis have all really come together in a way that makes a lot of sense. It’s almost too good to be true!’
This research was supported by grants from the Leverhulme Trust and the European Research Council awarded to Matthew Grubb.
About the Leverhulme Trust
The Leverhulme Trust was established by the Will of William Hesketh Lever, the founder of Lever Brothers. Since 1925 the Trust has provided grants and scholarships for research and education. Today, it is one of the largest all-subject providers of research funding in the UK, currently distributing £100 million each year. For more information about the Trust, please visit the website and follow the Trust on Twitter @LeverhulmeTrust.
Contact: Louise Pratt, Head of Communications, IoPPN: louise.a.pratt@kcl.ac.uk / +44 7850 919 020

