The first wave of COVID was a difficult time for us all; as researchers we were redeployed and at the frontline of the pandemic. All we could think about was doing the best for our patients. I was therefore taken by complete surprise two weeks ago when I received a phone call stating I had been selected from a large number of applications to be given this award which will enable us to continue to conduct our research into valve thrombosis.
Dr Tiffany Patterson, School of Cardiovascular Medicine & Sciences
15 September 2020
Dr Tiffany Patterson wins prestigious Josephine Lansdell Grant for research into heart disease
Dr Tiffany Patterson from the School of Cardiovascular Medicine & Sciences has been awarded the Josephine Lansdell Grant from the British Medical Association Foundation for Medical Research.
Dr Tiffany Patterson, NIHR Academic Clinical Lecturer in Interventional Cardiology in the School of Cardiovascular Medicine & Sciences, has been awarded the Josephine Lansdell Grant, totalling 65k, from the British Medical Association (BMA) Foundation for Medical Research.
The BMA Foundation for Medical Research is the oldest medical organisation in the world, awarding grants and prizes to encourage and further medical research since 1839. The Josephine Lansdell Grant is awarded just once a year, primarily to early-career researchers, and will be used to support Dr Patterson’s research into heart disease.
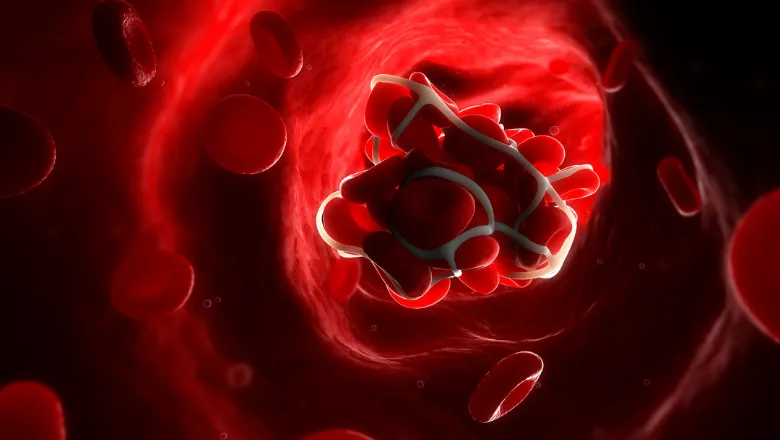
Dr Patterson joined King’s as a Clinical Research Fellow in 2012 and was awarded a British Heart Foundation Clinical Research Training Fellowship to study ischaemic heart disease. She received her PhD in 2017 on ‘Flow contraction matching in the human heart’. As her career has progressed, Dr Patterson has focused her interests on transcatheter heart valve durability and investigating the causes of early valve thrombosis – or clotting.
Aortic stenosis is one of the most common and serious heart valve disease problems, narrowing the aortic valves ability to open and ultimately restricting blood flow in the heart. The disease has a 50% mortality rate once symptoms develop, which is worse than most cancers.
In many cases of aortic stenosis, heart valve surgery is performed to replace the faulty or damaged valve. However, sometimes patients are not considered suitable to undergo the surgery and are offered a transcatheter aortic valve implantation (TAVI) procedure instead, which uses a catheter to fix a replacement valve.
While TAVI have revolutionised the treatment of aortic stenosis for many patients, it is still a relatively new procedure and its long-term benefits and risks are still being studied. Over the past two years, it has become apparent that up to 10% of patients have early signs of blood clot formation on their new heart valve.
While the presence of thrombosis would normally be treated with blood thinners, the aortic stenotic population are a high-risk group for bleeding due to multiple comorbidities. As such, it is essential to be able to predict, and therefore prevent, clot formation.
Dr Patterson aims to examine the haematological and anatomical variations that would suggest if a patient would be prone to developing clots on their heart valves.
I am of course very grateful to the BMA Foundation for Medical Research for recognising this clinical need and enabling us to answer our research question.
Dr Tiffany Patterson, School of Cardiovascular Medicine & Sciences
