25 September 2018
In Conversation With: Prof Terry Peters
King's welcomes Terry Peters, a Professor of Biomedical Engineering, Medical Biophysics and Medical Imaging and a Scientist at the Robarts Research Institute at Western University.
This September we are delighted to welcome Terry Peters to the School on a six-month sabbatical. Terry is a Professor of Biomedical Engineering, Medical Biophysics and Medical Imaging and a Scientist at the Robarts Research Institute at Western University in London Canada. Until last month he was also the Director of the Biomedical Imaging Research Centre (BIRC) at Western, and brings over 40 years of expertise in medical imaging to the School.
Read our interview to discover how the field has developed during his renowned career, what he will be working on at King’s, and what the next research breakthroughs in medical imaging might look like:
What made you choose the path of medical imaging as a career?
I was awarded my PhD in Electrical Engineering in 1974 from the University of Canterbury (Christchurch, New Zealand) producing the world’s first thesis on CT scanning, but it wasn’t until I went on to work for Christchurch Hospital that I got my real introduction to how medical imaging could make a difference. We convinced the hospital administration to invest ($20,000 NZD) in the construction of a CT scanner, which went on to be used clinically for radiotherapy treatment planning. At the time, this was very novel, cutting-edge technology, and preceded the first commercial CT at the hospital.
Because of my early exposure to CT scanning, the NZ government asked me to tour the US, Canada, and Europe to characterize and compare CT scanners, finally making recommendations for their introduction to New Zealand. During one of these tours, a turning point for my career came in the form of exposure to MRI technology at the International CT Conference (Stanford, 1975). A seminal paper on MRI was presented by Paul Lauterbur, who later shared the Nobel Prize in Physiology or Medicine in 2003 with Sir Peter Mansfield, which opened up my own research to innovative new ideas. At the same meeting, I met another New Zealander, Dr Chris Thompson, who was working at the Montreal Neurological Institute (MNI), and who invited me to spend 2 years there.
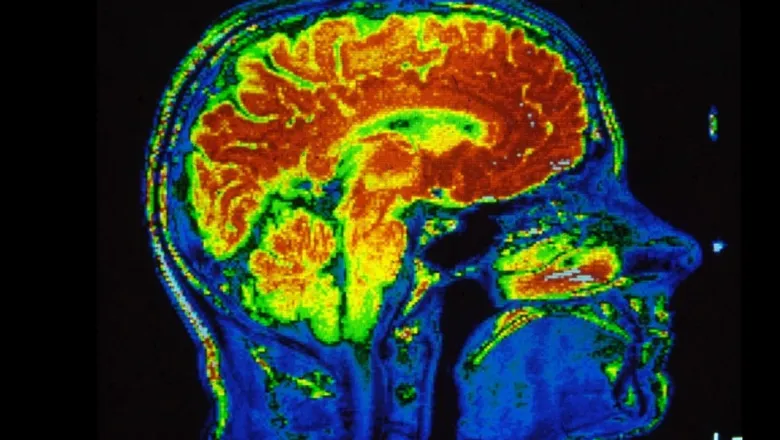
Two years became 19, and while at the MNI, I became an active member of the Neurology & Neurosurgery, Biomedical Engineering and Medical Physics Departments at McGill University where I explored the use of CT scanning in the brain in more depth, including 3D imaging, working with Neurosurgeons to develop image-guided neurosurgical planning. I was also responsible for introducing the first 0.5T “high-field” (yes, ½ Tesla magnets were considered high-field in 1984!) cryo-magnet MRI in Canada.
In 1997, the Imaging group at the Robarts Research Institute (RRI) at Western University asked me if I was interested in starting an image-guided surgery program in (the other) London in Ontario. This was where I established my lab, initially focussing on image-guided neurosurgery, then moving into other IGT disciplines such as cardiac and abdominal. This research group became the VASST (Virtual Augmentation and Simulation for Surgery and Therapy) Lab.
What have been the major research breakthroughs in medical imaging that you have seen?
A number of new technologies have disrupted the clinical practice since my first days as a medical physicist. When I first became excited about the fact that I could reconstruct images using CT principles, my radiology colleagues never thought this could replace X-Ray imaging. The same thing happened with MRI – by this point CT was well established in clinical practice and it was difficult to convince teams to accept yet another imaging modality. (Fortunately, they eventually changed their minds!)
The rate of tech expansion has always amazed me. MRI is the result of an incredible interaction between so many disciplines. These almost magical machines would never have materialized without such an enormous multi-disciplinary collaboration between chemistry, physics, electrical engineering, computer science, radiofrequency coil design, and cryogenics. Since that point we’ve been able to progress from acquiring single slices to dynamic volumes, capturing thousands of images in minutes.
What do you predict as the next big changes we will see in the sector?
I’ve always found that new breakthroughs are often things you can’t predict – the whole evolution of CT and MRI is indicative of this. We certainly didn’t predict we would be doing live functional MRI when things were starting. It just didn't seem possible.
Our work at Robarts, and here at the BMEIS School, is focused on minimally invasive surgery with dedicated, intelligent instruments, coupled with imaging to help us approach surgical targets more precisely and safely. I think we have tremendous opportunities to use developments in computing, robotics and artificial intelligence, along with imaging, to help us achieve these goals – and it’s absolutely essential that we work together.
A shift in the field is the way we’re using the latest technologies to develop more economic solutions to clinical practice. For example, Robarts has Canada’s only 7T scanner, but it would be impossible to expect to scan every patient who requires an MRI with this facility. However, with the advantage of the higher resolution and sensitivity offered by the 7T, we can identify characteristics of the brain which aren’t currently visible on lower field scanners, and this in turn informs us about how to improve protocols to extract similar information with the more widely available 3T machines.
Another example is the opportunity to use low footprint and affordable ultrasound, (whose quality has improved dramatically over the past couple of decades), combined with augmented reality visualization techniques, to develop low cost solutions for minimally-invasive therapies for widespread deployment in less developed countries.
What will you be focusing on during your sabbatical with the School?
I’m here to learn as much as I can. We’ve already started writing a joint grant between King’s and Western University concerned with using High Field imaging to better diagnose epilepsy by more accurately locating the signals we get from electrodes placed in the brain.
I also want to learn more about what’s going on in Deep Learning and if there’s a way we can use this approach to predict the histology of affected brain areas from MRI in epilepsy patients. At MICCAI, which took place just last week, there’s been a definite shift towards Deep Learning in medical image computing, and I’m particularly interested in how that can help the computer assisted image-guidance community. I’m planning to work closely with Prof Julia Schnabel, Chair in Computational Imaging, and her team to learn more about her work using Deep Learning to analyse MRI scans.
At Robarts, we also work a lot with cardiac interventions. I want to find out what techniques I can take back to Canada to understand heart valve pathologies using MRI imaging to help us design better therapies and treatments.
My lab also has an ongoing collaboration with King’s College Hospital at Denmark Hill on mitral valve repair, where we are creating patient-specific valve models to help understand the impact of new therapies.
On the other hand, I also hope I can bring some expertise from Robarts’ to the table. My colleagues already have 10 years’ experience with 7T MRI, developing new pulse sequences and building customized coils in their radiofrequency labs. This expertise will be of huge benefit when setting up the new 7T facilities at St Thomas’.
