About 18 years ago, we were the first to prospectively isolate and report the origins of MLL stem cells in mouse models. However, information regarding the treatment-resistant MLL-AML in humans is still largely missing, which has important implications in translating our findings to the clinic.
Professor Eric So, School of Cancer & Pharmaceutical Sciences
24 February 2021
Investigating the origin of acute myeloid leukaemia
New research identifies a potential novel therapy to overcome chemotherapy resistant cancer cells.
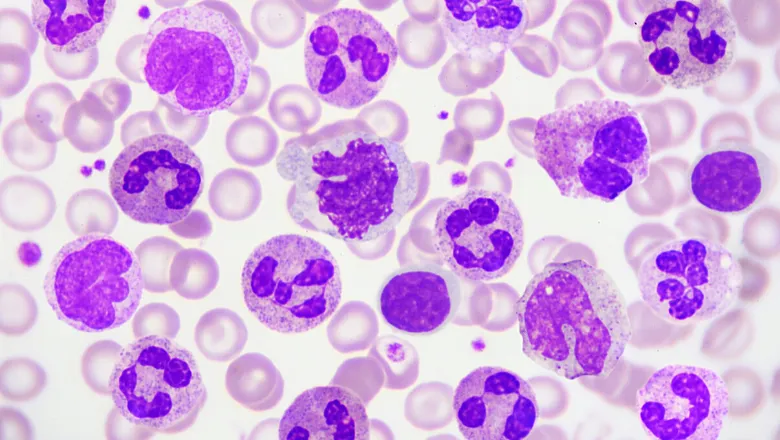
Leukaemia is a type of cancer that most often starts in early forms of white blood cells. Acute myeloid leukaemia (AML) means the cancer progresses rapidly and aggressively, attacking a specific type of white blood cell – referred to as myeloid cells – which are known to play a key role in fighting bacterial infections, defending the body against parasites, and preventing the spread of tissue damage.
AML carrying the MLL gene mutation (MLL-AML) is one of the most devastating cancers, with only a two-year survival rate of less than 25%. The major cause of treatment failure is because the cancer cells resist the effects of chemotherapy, which are believed at least in part due to the nature of the cells and their specific ways of interacting with the mutations. Therefore, it is paramount to characterize the origins and molecular features of these treatment-resistant cells.
To solve this issue, a team of researchers from the School of Cancer & Pharmaceutical Sciences, led by Eric So, Professor and Chair in Leukaemia Biology, have remodelled the human AML disease, with support from Cancer Research UK and Blood Cancer UK.
For the first time, researchers have identified normal blood stem cells, but not their more mature downstream progenies, as the origin of treatment-resistant AML stem cells, which drive and sustain the disease. By further analysing the cells' molecular characteristics, the team were able to reveal the presence of a particular multidrug-resistant pump.
By targeting this pump with an antibiotic currently used in the clinic for diarrheal disease, researchers were able to sensitise the AML cells to chemotherapy treatment and significantly extend survival rates in disease models carrying the human MLL mutated AML cells from patients.
Since the antibiotic, Fidaxomicin, is currently available, a small clinical trial would be the next logical step to translate our findings to the clinic. On the other hand, our new humanised models can also provide a novel platform to characterise and further identify potential new targets for effective treatments.
Professor Eric So, School of Cancer & Pharmaceutical Sciences
Read the paper in Science Translational Medicine.
