We uncovered that if you look at the scarring on these patient’s hearts, which is present in about a third of these patients, and if you trace around the perimeter of that scar, then that is the biomarker we’re looking for that you can measure and quantify.
Dr Martin Bishop
30 October 2020
Novel biomarker and modelling could help better identify lethal arrhythmias
Novel biomarker and computational modelling could lead to better identification of heart arrhythmias
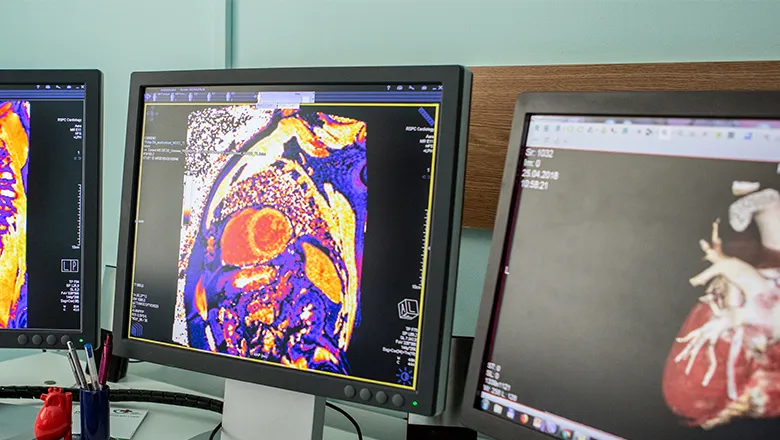
Researchers at the School of Biomedical Engineering & Imaging Sciences at King’s College London, in collaboration with colleagues at the Royal Brompton & Harefield NHS Foundation Trust, have identified a novel imaging-biomarker that can be used to help differentiate risk levels of lethal arrhythmias (irregular heartbeat) in patients with problematic left ventricles. For the first time, they have used detailed computational modelling to also understand why this biomarker is important, in the hopes it will help clinical translation and personalise medicine.
Published today in JACC: Electro Electrophysiology, the researchers also showed that patient-specific computational simulations alone could be used as a predictive tool to identify individual risk of arrhythmias. This is the first-time modelling has been used in this manner on such a large (>150 in this case) patient cohort.
Making the decision as to whether to input defibrillators in these patients is very difficult with the current tools that clinicians have.
It is known that current metrics used are inadequate and outdated, yet they are still widely used as there has not been strong enough evidence against it.
Lead researcher Dr Martin Bishop said there are still large numbers of these patients that die because they have not been identified as being high risk. Similarly, there are many patients that have been given devices when they are not needed.
“This costs a huge amount of money to the NHS and the devices have their own side effects and long-term consequences, so you really need to be making this decision as correctly as possible,” he said.
Dr Bishop said clinicians would be looking for new clinical methods that are non-invasive such as cardiac MRI images to locate potential anomalies.
Dr Bishop said as the clinical study only provides an empirical result, it therefore does not explain why the biomarker is important.
Therefore, in tandem to the imaging biomarker the researchers used quite detailed computational simulations, also known as ‘digital twin’ simulations, to try to use them to understand that biomarker.
The main novelty in the study is combining the biomarker with modelling on a significantly sized cohort. It means the modelling on its own is a lot more predictive than a lot of the clinical tools.
“This means that a patient can come in, have a scan and the clinician would be able to make a model of your heart based on that scan,” Dr Bishop said.
"Clinicians can do some simulations and that can be more predictive on its own than a lot of the clinical tools that are currently being used – that’s patient specific personalised medicine.”
In the future the methodology could be applied on larger cohorts and for other types of disease.
"This is the most interesting next step and that is something that we’re currently working on with our existing collaborators,” Dr Bishop said.
The research is funded by the Medical Research Council (MRC).
