If we could achieve a high imaging quality that could be provided to the surgery it would reduce complications such as nerve damage.
Mengjie Shi, PhD student, School of Biomedical Engineering & Imaging Sciences
31 May 2022
Novel deep learning technique developed for photoacoustic imaging technology
The system is designed to improve visualisation of immersive medical devices during minimally invasive procedures

A postgraduate student from the School of Biomedical Engineering & Imaging Sciences has developed a deep learning framework to enhance a novel light emitting diodes (LED) based photoacoustic imaging technique to improve visualisation of immersive medical devices during minimally invasive procedures.
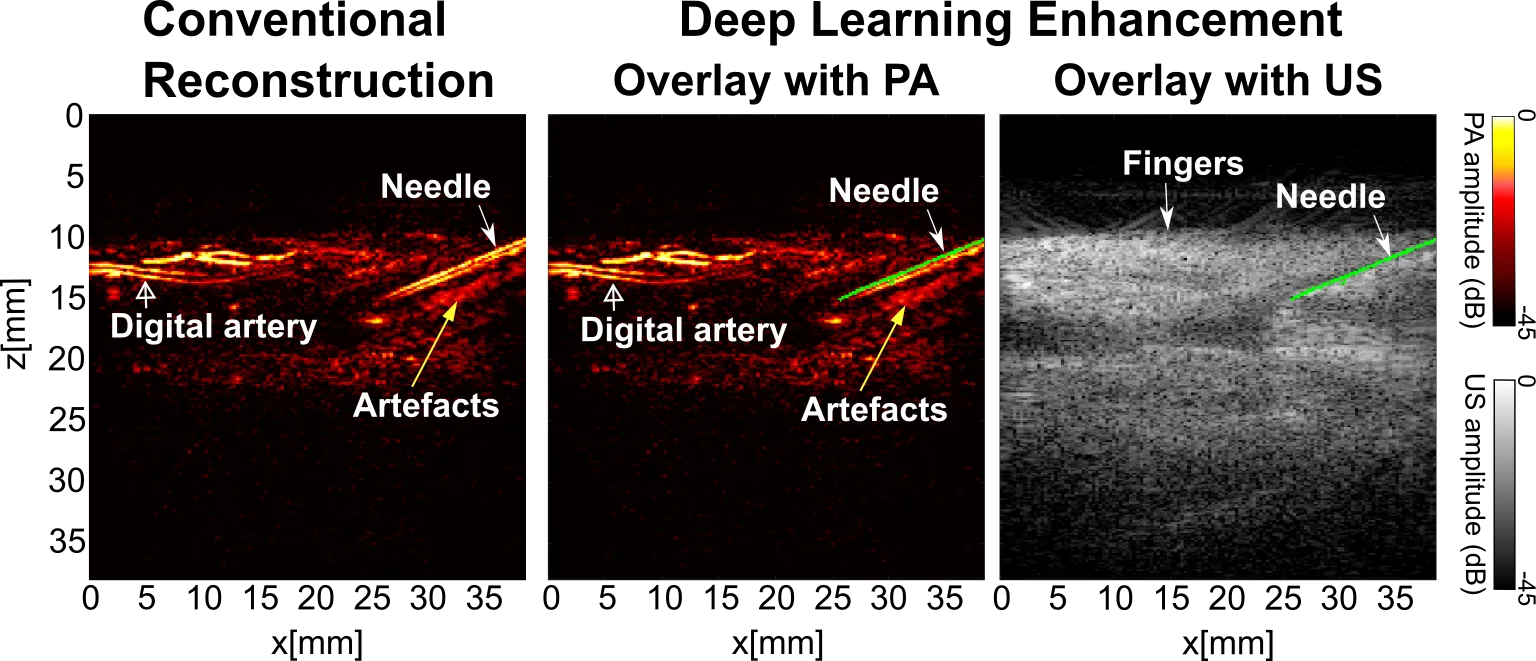
The paper, published in Photoacoustics demonstrated that the learning-based framework substantially improved the needle visibility in photoacoustic imaging in vivo compared to conventional reconstruction by suppressing background noise and image artefacts – meaning the images were much clearer and provided better visualisation of the needle.
The researchers say the proposed framework could be helpful for reducing complications during percutaneous needle insertions – procedure or method where access to inner organs or other tissue is done via needle-puncture of the skin, rather than by using an "open" approach where inner organs or tissue are exposed – by accurate identification of clinical needles in photoacoustic imaging.
Ultrasound (US) imaging is widely used for guiding minimally invasive percutaneous procedures such as peripheral nerve blocks, tumour biopsy and fetal blood sampling.
During these procedures, a metallic needle is inserted percutaneously into the body towards the target under real-time US guidance. Accurate and efficient identification of the target and the needle are of paramount importance to ensure the efficacy and safety of the procedure.
Photoacoustic imaging is a hybrid modality that is based on the detection of US signals generated from tissue in response to tissue absorption of light.
As each type of tissue has absorption preference for certain colours of light, photoacoustic imaging can differentiate various tissue types at high spatial resolution, which could help surgeon to better identify procedure targets and avoid damaging critical tissue structures.
First author and PhD student Mengjie Shi at the School of Biomedical Engineering & Imaging Sciences said as the framework has been validated on healthy human volunteers, it can be integrated into real-time applications. This can give clinicians real-time feedback of the needle position so they can approach the needle to the procedure target with high confidence as they receive feedback from the photoacoustic images and US images to conduct better procedures.
The researchers say it could also work well in a clinical environment as LED is safer and more cost-effective compared to commonly used bulky and expensive laser systems. Light-emitting-diodes (LEDs) are one of low-cost alternatives to solid-state lasers. PA could use different light sources for light excitation such as solid-state lasers, laser diodes, and LEDs. Here, LEDs are promising alternatives for their compact size, low cost and safe operation.
This means surgeons and clinicians may not need to wear goggles to protect their eyes from the laser’s radiation. For LED-based photoacoustic imaging systems, only two pieces of LED arrays and cables are needed.
With these two factors in mind, clinical translation of this photoacoustic imaging technique could be accelerated.
Dr Xia, Lecturer, Department of Surgical & Intervention Engineering, School of Biomedical Engineering & Imaging Sciences
This research adds to their work showing how photoacoustic imaging is optimizing and merging hybrid imaging modalities that could be used for guiding minimally invasive procedures.
