There is a rising tide of polypharmacy in rheumatoid arthritis patients who are prescribed combination strategy medications for their arthritis. This is often in addition to drugs used for symptoms control and management of other comorbid diseases. The publication of this work will help highlight to clinicians the impact of polypharmacy on clinical outcomes in rheumatoid arthritis. It should also empower patients to discuss the number of medications they take with their primary care physicians or rheumatologist. This work supports the use of a medication count as a valid tool in clinical research.
Lead author of the study Dr Katie Bechman
17 April 2019
Patients prescribed multiple medications have worse outcomes in Rheumatoid Arthritis
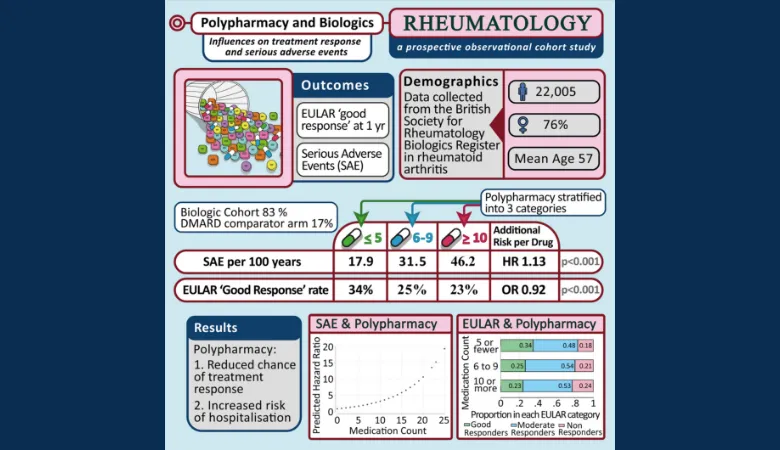
Research published in Rheumatology has found that polypharmacy is associated with poorer clinical outcomes for patients receiving treatment for rheumatoid arthritis.

Polypharmacy is the simultaneous use of multiple medications by a patient. It is becoming more common, with over half of patients over 65 prescribed five or more medications.
Patients with rheumatoid arthritis are prescribed medications to manage their arthritis, to control pain and to counter side effects of certain drugs. This is often in addition to the medications used to manage other diseases that occur alongside their rheumatoid arthritis. Authors of this paper are suggesting that the number of medications a patient is prescribed could be used as a marker of their health.
The aim of this research was to assess if polypharmacy is associated with poorer outcomes for patients receiving treatment for rheumatoid arthritis. The authors examined 22,005 patients with rheumatoid arthritis who were registered to the British Society of Rheumatology Biologics Register (BSRBR-RA). The BSRBR-RA is a large observational cohort, established in 2001, to monitor the long-term safety of biological therapy prescribed for rheumatoid arthritis. Biological therapies target key chemicals that drive inflammation in rheumatoid arthritis. By blocking these chemicals they reduce joint pain, swelling and damage. These therapies improve the symptoms of rheumatoid arthritis for many patients.
The authors found that the average number of medications prescribed in addition to their biologic therapy was five, with the greater number of drugs at 25. 7% of patients were prescribed more than 10 medications.
Their findings also show that for each additional medication a patient is taking, they are 8% less likely to achieve a good treatment response when starting a biologic. Additionally, each additional medication prescribed was associated with a 13% increased risk in having a serious adverse event that required hospitalization, for example, an infection.
Based on these findings, it is possible for physicians to use a patient’s medication count as an indicator of how well they may respond to biologic therapies and their risk of possible complications.
The next steps in this research are to further analyse the BSRBR-RA dataset to identify if any particular types of drugs, for example, those prescribed for cardiovascular disease are associated with worse clinical outcomes.
