In our biological device, nerve-muscle connections strengthen with training, similar to the effect of exercise on human muscle. This model resembles real neural circuits more closely than conventional cultures systems and has a better chance of capturing early stages of neurological diseases, such as ALS.”
Dr Ivo Lieberam, Centre for Stem Cells & Regenerative Medicine
20 May 2019
Researchers develop new method to understand ALS
King’s scientists have developed an alternative way to investigate the breakdown in connection between muscles and the brain for sufferers of ALS.
Amyotrophic Lateral Sclerosis (ALS), also known as motor neuron disease, is a medical condition that affects the cells which connect the brain to muscles, called motor neurons. ALS suffers lose control of their muscles and this can eventually lead to paralysis, meaning the affected individuals can no longer walk, speak or breathe.
The disease progressively gets worse over time and is currently incurable, therefore many scientists study its causes and possible therapies.
Investigations of ALS cannot be carried out in patients and can only be done so with experimental animals, mostly mice and rats. The animals are often genetically modified such that they develop a disease which is like ALS in humans. This approach uses large numbers of animals, is expensive and time-consuming, and therefore not ideal to systematically study the causes of the disease.
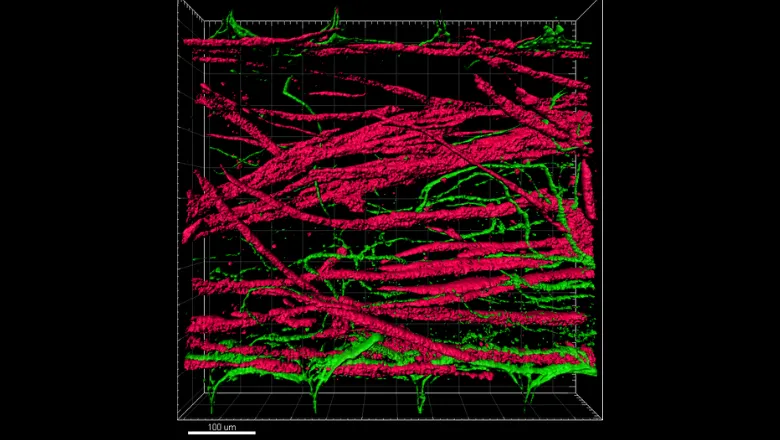
King’s scientists, in collaboration with the National University of Singapore, have developed an alternative way of investigating the connection between the brain and muscle, and its decline in ALS. Their model, called ‘motion in a dish’ is based on artificial tissues resembling nerve and muscle tissues grown directly from stem cells.
The device mimics the human system by having nerve and muscle tissues connected by motor neurons however they have been genetically engineered to carry optical probes which allow researchers to transmit instructions to them with light flashes.
The team validated their model in two different ways; firstly, they activated the nerve-muscle circuit with light over several days and observed that this strengthened the connections between motor neurons and muscle fibres, as it does in humans. Secondly, they showed that a genetic defect associated with ALS in humans caused the degeneration of nerves and the loss of connections between nerves and muscle fibres. They were able to reverse these effects with Necrostatin, a candidate ALS drug.
The next steps for this model are to investigate how some people are protected from developing ALS by their genetic makeup and how such protection may be mimicked with drugs. The authors believe this model will allow scientist to discover new ALS drugs faster, cheaper and without the use of animal experimentation.
Read the full publication here.
