04 September 2020
Researchers develop novel way to better detect disease in the heart
The team has identified a clearer with which to identify disease

In a preliminary study, researchers from the School of Biomedical Engineering & Imaging Sciences have developed a method to produce whole-heart quantitative MRI images by mapping properties in the heart to detect disease more clearly and accurately.
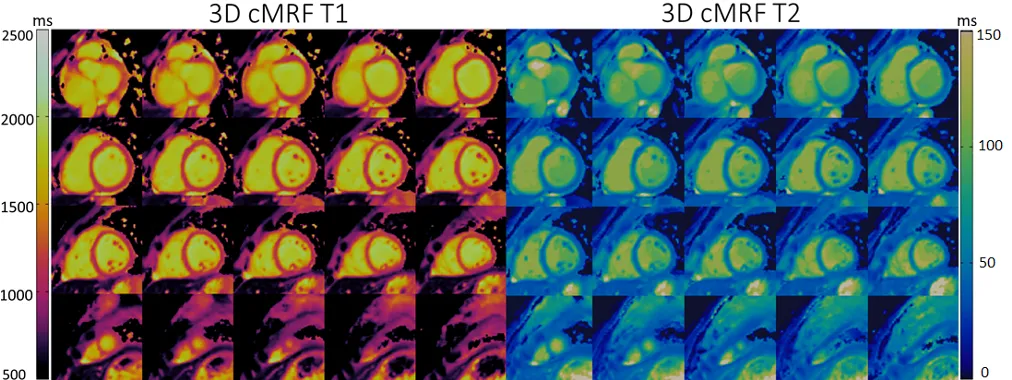
Published in NMR in Biomedicine, the study from Dr. Gastao Lima da Cruz, part of the research team led by Dr. Claudia Prieto in collaboration with Prof. René Botnar, is devising a technique to allow for whole heart mapping of the parameters T1 and T2, which associate each image pixel with two numbers that directly connect with biological properties of tissue. This way, it becomes very clear for a clinician to detect and analyze disease.
“Most MR images that are performed are qualitative, meaning that a radiologist looks at the image to see if a part of the tissue is maybe a bit darker or brighter (hypo or hyper intense) than it should be,” Dr. Cruz said.
“What we’re trying to achieve is something refer to as myocardial tissue characterization. If you can measure the tissue properties of the heart muscle (e.g. T1 and T2), you can identify sickness in each part of the muscle. This way, you can not only describe the type of disease, but also determine how sick the heart muscle is – from being completely healthy to being beyond repair.”
“One way to achieve this is exactly by measuring these fundamental parameters or biomarkers. If we can characterize the whole-heart tissue then we can very accurately diagnose and sometimes even predict future disease in the heart.”
Compared to other modalities like X-Ray or CT which are very fast modalities, one of the main limitations of MRI is that it is very slow.
An MRI scan usually takes anywhere between 30-60 minutes and often involves multiple scans. While most MR scans are acquired in the order of a few minutes, this is enough to cause problems due to motion from breathing and beating heart.
Patients may therefore be asked to hold their breath during a scan, however in many cases the patient is not capable of doing so. Long scan times also mean that these T1 and T2 parameters are usually measured for a single slice across the heart, instead of covering the entire heart. Furthermore, these parameters are usually measured in two sequential scans, whereas with type of sequences both parameters can be estimated from a single scan.
The researchers have demonstrated that this new method allows for the correction of respiratory motion in a free-breathing scan, allowing for simultaneous 3D whole heart images of T1 and T2 parameters.
“The findings show that this is a feasible technique that we can deploy in the future and we can achieve a 3D volume of the T1 and the T2 of the heart using free-breathing acquisitions, which is very promising for future developments,” Dr. Cruz said.
“The benefits of this framework are three-fold across the entire clinical pipeline. It’s easier for the patient, easier scanning for the radiographer and easier analysis for the cardiologist.”
For patients, the scan time is reduced, and the number of scans as well. Moreover, no breath-holds are required which is challenging and even impossible in some patients.
Radiographers, who manage these scans would have to plan for only one scan, where previously, if they wanted to acquire the T1 and T2, and even several slices of the heart to obtain full coverage, they would have to plan multiple scans to gather different data sets.
As this new method requires one scan that can give you the entire 3D picture in one scan, cardiologists can now have important information embedded into one dataset, so everything is co-registered and aligned.
“Before, cardiologists would have had all these images that require different breath holds and were maybe not aligned because the patient was struggling. Now it all comes from one 3D volume and it’s very easy for the cardiologist to analyse”.
In the future, the researchers are looking to map even more parameters from a single scan, which will further help identify underlying disease.
“From one scan we can get all this multi-parametric information and together it helps distinguish between different diseases. As we incorporate more parameters, we’ll be able to perfectly pinpoint what is the disease, how far advanced it is and what the recommended treatment options are.” Dr. Cruz said.
