This then begged the question: how can countries establish benchmarks for developing their national cancer surgery plans?
Professor Richard Sullivan
12 February 2021
Researchers examine how countries establish benchmarks for developing their national cancer surgery plans
Understanding the differences in cancer care and surgery across the world is key.

One of the most critical research issues for national and global cancer policy is to understand which gaps exist in human resourcing of cancer surgery. To address the skill shortages that certain countries may have, and the support in up-skilling or training that they may need, this needs to be comprehensively investigated.
With this aim in mind, a team of researchers from the School of Cancer & Pharmaceutical Sciences, led by Professor Richard Sullivan, have started a collaboration between the Institute of Cancer Policy, of which Richard is a Director at, and a group at the University of New South Wales – led by Professor Michael Barton. Professor Barton’s team had previously developed methodologies for looking into this critical health systems issue.
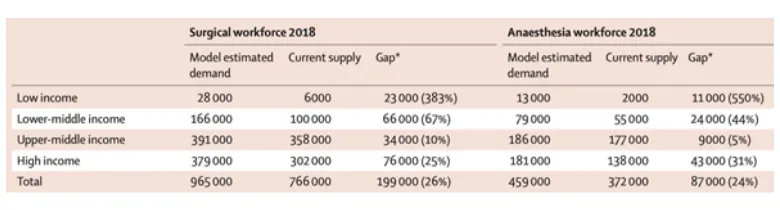
Their initial analysis revealed that there are massive workforce deficits in low-middle and low-income countries, because there is not sufficient training for enough surgical staff, as well as an inadequate expenditure of health, lack of surgical centres of excellence and, a lack of cancer surgical clinical trials. It was also found that there is significant migration of trained surgeons to the higher income countries.
The team created a tool, using Australian data, that allowed them to benchmark whether too little, or too much surgery was being performed in each country. The table below shows site specific cancers benchmarked against what was expected, and what the researchers revealed.
Cancer surgery is at the heart of modern management of cancer, and an absolutely crucial determinant of better, more affordable and high-quality patient outcomes. But many countries, as we know, have significant deficits. Understanding the magnitude of these deficits and providing validated tools for national cancer surgical planning is a foundational aspect of building better cancer surgical care.
Professor Richard Sullivan
The huge gaps in the provision of surgical and anaesthetic workforce for cancer control are massive hurdles to Universal Health Coverage for cancer, and other global initiatives such as Elimination of Cancer of the Cervix and the Global Breast Cancer Initiative. Creative solutions and more capacity funding for the cancer surgical workforce are needed, particularly from overseas development assistance to help mitigate the additional impact of the post COVID pandemic economic downturns.
Read both the papers here:
https://www.thelancet.com/commissions/global-surgery
https://www.thelancet.com/journals/lanonc/article/PIIS1470-2045(15)00223-5/fulltext
