For many patients whose hope to restore their vision rests on emerging therapeutics, this research will mean a quicker and safer development cycle that will lead to the treatments becoming available sooner.
Dr Jack Lee
17 December 2020
Researchers to resuscitate eyes, speed up clinical research for vision impairment
An international consortium of researchers is developing a new method to bring eyes back to life from deceased body donors for clinical research purposes.
Researcher in the School of Biomedical Engineering & Imaging Sciences, Dr Jack Lee, is part of an international consortium of researchers developing a new method to bring eyes back to life from deceased body donors for clinical research purposes.
Coordinated by Pia Cosma at the Centre for Genomic Regulation (CRG) in Barcelona, the group is creating a device that resuscitates eyes from the dead.
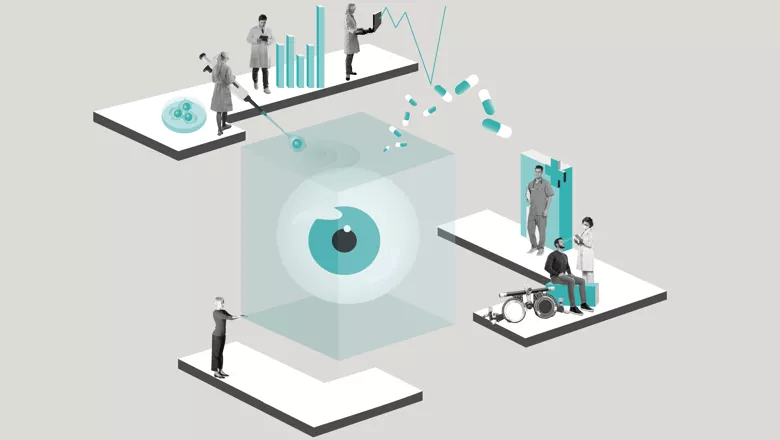
The device, codenamed ECaBox, will be a transparent, cubic box that mimics conditions in the living human eye, maintaining the eye’s temperature and pH levels while avoiding blood clots and removing metabolic waste and toxins.
Inside the ECaBox will be donor human eyeballs. The immediate goal is to test novel stem cell therapies without fear of risking patient harm on this platform.
Artificial blood will also be developed to provide cells with oxygen and nutrients, kick-starting the activity of nerve cells and restoring total eye function. Artificial vitreous humour will maintain the eye’s ocular pressure.
The health of the eyeball will be continuously monitored to confirm retinal function and regeneration. Beyond this scope, this technology can be extended to keep donor eyes intact for transplantation purposes, extending the current 48-hour window limit.
“King's College London will offer their expertise on computational modelling of perfusion and microvascular physiology to achieve optimal device operating parameters for the preservation of the eye,” Dr Lee said.
Vision impairment affects over 250 million people worldwide, with thirty-six million people being blind. Retinal degeneration is often incurable, and ageing populations worldwide are major social and economic challenges.
Current technological limitations mean that eyes can only be kept at 4ºC for a period of 48 hours before irreversible degradation. This greatly limits their use for experiments, particularly to test the effectiveness of new drugs and treatments.
While advances in human organoids, growing tissues in a petri dish, are successfully mimicking the function of the eye, they fail to encapsulate the eye’s physiological complexity, such as its immune, vasculature, and metabolism systems.
Pia Cosma, ICREA Research Professor and Group Leader at the Centre for Genomic Regulation (CRG) and coordinator of the project said: “There are a huge number of potential new treatments and therapies for eye damage and vision loss, but the eyewatering cost of running a clinical trial can mean they never reach the market.”
Our new method can greatly improve the preclinical validation steps for these treatments, supporting the screening of a larger number of candidates and helping promising drugs escape the ‘valley of death’ imposed by cost-benefit analyses in the pharmaceutical industry.
Pia Cosma, ICREA Research Professor and Group Leader at the Centre for Genomic Regulation
An early prototype of the device is expected to be built by end of 2023. Upon completion, the group plans to use the device to test their own retinal regenerative therapies pioneered at the CRG.
ECaBox will be created by an interdisciplinary collaboration between seven research centres. In Barcelona, the project will be coordinated by Pia Cosma at the CRG in collaboration with two other Catalan centres – Ricardo Casaroli at the Universitat de Barcelona and Nuria Montserrat at the Institute for Bioengineering of Catalonia (IBEC).
International collaborators include the Association for the Advancement of Tissue Engineering and Cell Based Technologies & Therapies (A4TEC) in Portugal, AFERETICA in Italy and the Bar-Ilan University (BIU) in Israel.
The project has been awarded 3.5 million euros by the European Union’s Future and Emerging Technologies Open research programme, which funds radical new technologies.
