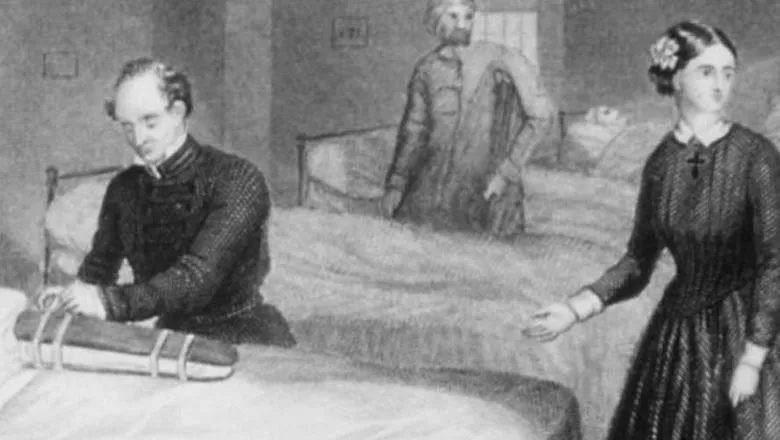
This ‘lady with the lamp’ – a moniker she earned while tending to the war wounded at the hospitals she helped to set up at Scutari during the Crimean War – set a new model for the good nurse: not just caring and vigilant, but also bureaucratically savvy, tough and unrelenting in her advocacy for both nursing and for her patients. Far more human than our collective nostalgia for her has made her seem, she was not the vision of beneficence and virtue some have made her out to be. But Florence Nightingale was always constant in her ability to get things done.
Here, out of the imposition of standards and rational design, sprung the modern healthcare system we have since embraced.
Like many of her generation, Nightingale only slow came to embrace germ theory, an idea that developed at the same time as her career over the 19th century. Instead she subscribed, as many at the time did, to a theory of contagion that saw illness as the result not of bacteria or viruses, but more primarily of ‘bad air.’
The reforms of sanitation that this drove were critical, showing themselves more essential to health improvement than were the bewildering array of cures and treatments for disease then on the medical market. Her healing system, the one she put in place in the war hospitals of the Crimean War, was indeed predicated on cleanliness, proper ventilation and nutrition and surveillance and tracking.
For Nightingale, saving lives was not necessarily about administering the right drugs at the right times. Instead, it was about maintaining the best possible conditions in which a body could heal itself. Indeed, the wards that she pioneered, and which continue to bear her name at some hospitals in the UK, bore the hallmarks of this belief system. They were large, open spaces - well-ventilated and clean - with heating and cooling systems designed to keep air swiftly circulating.
Later iterations saw the inclusion of under-bed ventilation systems, which created for each bed’s occupant their own personally ventilated space. Each ward was overseen by the nurse in charge, who could, at a glance, take stock of the entire space, triage those who needed closer observation and attend to those in trouble.
Though her views on contagion quickly became unfashionable in the twentieth century, in the 1970s a collection of medical critics engaged with Nightingale’s convictions that medicine was often ineffectual and almost always woefully disorganised, and that the body primarily needed space and conditions conducive to healing.
These critics, dismayed by what they saw as the shocking lack of efficacy of modern medicine and impressed by what the body could do on its own, also wondered whether the bedrock of medical care to be found not in good doctoring, but in good nursing: the creation of the right conditions for healing and the careful and attentive tracking of that healing over time.
Though we have almost completely dispensed with this view, opting instead for an extremely interventionist model of medical care - such that everything can be fixed if we can only find the right drugs, the right mix of chemicals, the right procedure, the right technology – we would do well to bring Nightingale’s ideas and approach back to the fore in our current pandemic.
And she, as others at the time, began to think epidemiologically about disease: creating data systems to standardise how deaths were recorded, for example, in order that comparisons could be more easily made.
This penchant for efficiency transformed not only nursing but healthcare itself. She would be impressed by the prominent leadership roles played by nurses in the pandemic and appreciative of the alacrity with which the emergency hospitals that bear her name were set up, though perhaps less thrilled about their ultimate inefficiency in service.
But she would have been dismayed by the bungling of the PPE supply chain and the lack of strategy to deploy testing to plan and manage the pandemic. These were aspects of healthcare she had sought to fix in her own time. She would be disappointed to see we had not yet learned this lesson.
In this moment where our health care system looks quite a lot more than we would like to admit like the Victorian system in which she worked, and where the bureaucratic ‘nonpharmaceutical interventions’ as we now call them – of the quarantining, tracking, and supportive care kind – have emerged once more as the critical treatment for what ails us, we could really use a Nightingale. Someone to speak truth to power and to get the job done.
For more information on the Bicentenary, click here