This work opens the 7T’s cutting-edge imaging modality to our most vulnerable patients. Our multidisciplinary approach focused on both extending the conditionality of specific anaesthetic equipment and monitoring to 7T alongside developing a wider clinical framework and environment. This ensures that ultra-high field scans under general anaesthesia are as medically relevant and safe as those acquired at usual lower clinical fields within the Evelina London Children’s Hospital.”
Dr Benjamin Blaise, Consultant Paediatric Anaesthetist, Evelina London Children’s Hospital, Guy’s and St Thomas’ NHS Foundation Trust, Senior Lecturer, Centre for the Developing Brain
22 March 2023
World first 7T MRI scan under general anaesthesia
For the first time, a patient has been scanned under general anaesthesia in the highly powerful MAGNETOM Terra 7T MRI scanner from Siemens Healthineers.
This new anaesthetic procedure will provide access to the 7T MRI scanner to patients who are unable to stay still in the scanner, such as young children. It could particularly help children with epilepsy, tumours and movement disorders which cause muscle spasms (dystonia) and also help drive innovative research projects.
The world first was completed in King’s College London’s Advanced MRI Centre, located St Thomas’ Hospital, London, and part of the Guy’s & St Thomas’ NIHR Imaging Clinical Research Facility. It provides a facility for researchers from leading research institutions in the capital to work together.
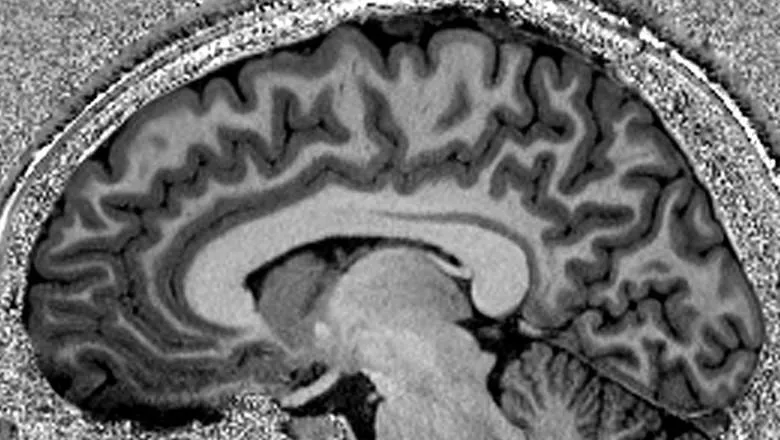
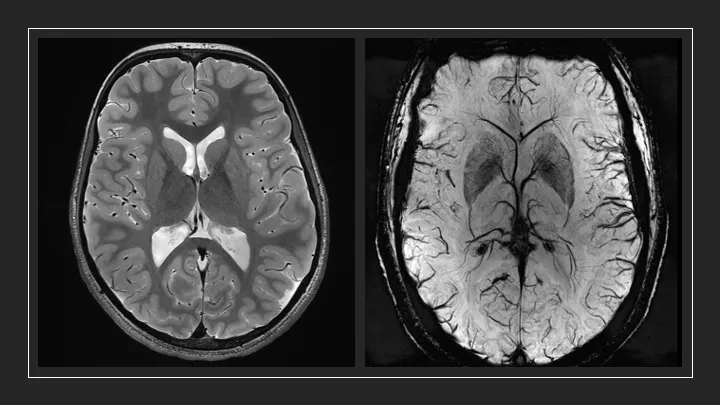
Some neurological conditions such as complex epilepsy and childhood epilepsy don’t show up well on some MRI machines. However, using the stronger magnetic field of the Terra system can allow more detailed pictures to be taken, leading to better visualisation of subtle brain abnormalities.
This can make it possible for patients to receive targeted treatment which greatly reduces symptoms.
We are delighted to have reached this major milestone of carrying out the first 7T clinical brain scan under general anaesthetic. This project has been a multi-disciplinary collaboration between clinical, academic and scientific staff at King’s and Guy’s and St Thomas’, with excellent support from industry partners. We now plan to offer this highly specialist service to suitable patients from all over the country, and are working with commissioners to realise that ambition.
Dr Sharon Giles, Director of Clinical & Research Imaging Operations, School of Biomedical Engineering & Imaging Sciences
The scanned patient suffers from epilepsy and had no lesions identified on their 3T MRI scan and different drugs did not stop their seizures.
The scan in the 7T went smoothly and the patient could go home on the same day.
This major achievement displays the power of collaboration between academia, NHS and industry – the three guiding pillars of our School which have allowed the successful delivery of this world first.
Professor Sebastien Ourselin FREng, Head of School, School of Biomedical Engineering & Imaging Sciences
The success of the world-first scan means the clinical team will be able to accept clinical referrals for patients requiring general anaesthetic, and research studies of vulnerable patients who might require anaesthetic intervention, can be supported.
One research study investigating MRI planning before insertion of deep brain stimulators (DBS) is now ready to start.
Preparatory works over two years included a testing programme developed with industry partners to determine the safe conditions of usage for anaesthetic and physiological monitoring equipment at 7T.
The scan was facilitated through a collaboration between the King’s Imaging team, the anaesthetic department from Evelina London Children’s Hospital together with colleagues across Guy’s & St Thomas’ NHS Foundation Trust, Philips Healthcare – MR patient monitoring and Dräger – MR anaesthesia workstation.
The team has also been awarded a GSTT ‘Learning from Excellence’ Award for the teamwork that allowed the first scan.
Notes:
This work was supported by a Wellcome Trust Collaboration in science award [WT201526/Z/16/Z], by core funding from the Wellcome/EPSRC Centre for Medical Engineering [WT203148/Z/16/Z] and by the National Institute for Health Research (NIHR) Biomedical Research Centre based at Guy’s and St Thomas’ NHS Foundation Trust and King’s College London and/or the NIHR Clinical Research Facility.
Clinical costs were supported by the Anaesthetic and Neurology Departments at the Evelina London Children’s Hospital.
