Nurturing and Empowering future parents through Support and Treatment (NEST)
People with mental health problems may find it hard to decide when and how to have children. People want to be in the best possible health when they get pregnant but for those with mental health problems there may be difficulties. This includes future fathers as well as mothers.
Work package 1 (realist evaluation)
What current model(s) of pregnancy planning support in mental health services, for those of reproductive age, can best facilitate decision making about planning and fitness for pregnancy and in what circumstances?
Realist evaluation approach involving focus groups and semi-structured interviews with clinicians and patients across selected mental health services (South London and Maudsley NHS Foundation Trust and Cumbria, Northumberland, Tyne and Wear NHS Foundation Trust), alongside routinely collected data on service use, to generate a programme theory of optimal pregnancy planning support in mental health services.
Summary for those without scientific/academic background: we will talk to people with mental health problems and the doctors, nurses and other people who support them with their mental health in South London and the North East of England. We will also look at the notes made about them by those supporting them. This will tell us if and how they are getting help at the moment.
Work package 2 (co-designing intervention(s))
What shared decision-making tool is needed to enable mental health services to support planning and fitness for pregnancy and is this feasible and acceptable among clinicians and patients?
Using the programme theory from work package 1 to inform the co-design of an intervention to support health and wellbeing in the context of planning and fitness for pregnancy, for use in mental health services. Using qualitative methods, acceptability, appropriateness and feasibility of the tool will be assessed.
Summary for those without scientific/academic background: we will work with people with mental health problems and those who support them. Together we will develop a way of helping people with mental health problems to make decisions about how they can improve their health.
The people supporting them can help them with this. It may be that they do not want to become a parent any time soon. Perhaps instead they would like advice on how to prevent pregnancy. It may be that they want help with stopping smoking so that they are healthier when they do decide to have children.
Some people may want advice about what might happen to their mental health problem when they become a parent. Other people might be unsure about how the medication they are taking could affect their chances of becoming pregnant. We will work with people with mental health problems from different backgrounds to make sure that they are getting the help that they need.
Work package 3 (pilot feasibility trial)
In mental health services, how feasible is a future effectiveness trial of the co-designed intervention?
Cluster randomised feasibility trial will assess feasibility of an effectiveness trial across mental health services in South London and the North East utilising routinely collected data and focus groups with clinicians.
Summary for those without scientific/academic background: we will ask people with mental health problems and those supporting them if the help that we have developed is useful to them.
We will also look at their notes to see if people with mental health problems are talking about these issues mentioned above when they are being supported with their mental health. We will also look at whether or not other people and health services have been asked to help them; for example social workers and nurses that help with cutting down on alcohol.
The research will tell us how we can help people with mental health problems get ready for when they have a baby. If they don’t have a baby, they will still be helped with getting healthier. We will share what we have learnt with people with mental health problems across the UK, those who support them and the Government.
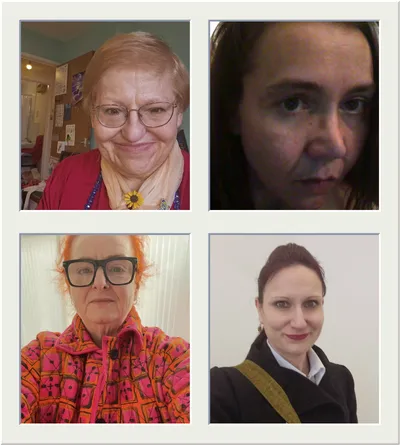
NEST Lived Experience Group
External Collaborators
- Alkis Velivasis, North London NHS Foundation Trust
- Chris McCree, South London and Maudsley NHS Foundation Trust
- Claire Smiles, Newcastle University
- Clevanne Julce, University of Massachusetts Amherst Chan Medical School, USA
- Danielle Schoenaker, University of Southampton
- Eleanor Swift, Mersey Care NHS Foundation Trust
- Emily Finch, South London and Maudsley NHS Foundation Trust
- Everyturn Mental Health
- Geoff Wong, University of Oxford
- Janine Smith
- Jenny Hall, University College London
- Joanne Butler, South London and Maudsley NHS Foundation Trust
- Justine Cawley, East London NHS Foundation Trust
- Michelle Howard
- Monica Franklin, NHS South East London Integrated Care Board
- Philipa Greenfield, Camden and Islington NHS Foundation Trust
- Polly Cohen, University College London
- Rowena Murray-Park, Cumbria, Northumberland, Tyne and Wear NHS Foundation Trust
- Ruth McGovern, Newcastle University
- Scott Mair, Fatherhood Solutions

Principal Investigator
Affiliations
Funding
Funding Body: NIHR
Amount: £817,432
Period: September 2024 - September 2028

