POPS-SUp
Implementation of Comprehensive Geriatric Assessment based perioperative medicine services to improve clinical outcomes for older patients undergoing elective and emergency surgery with cost effectiveness
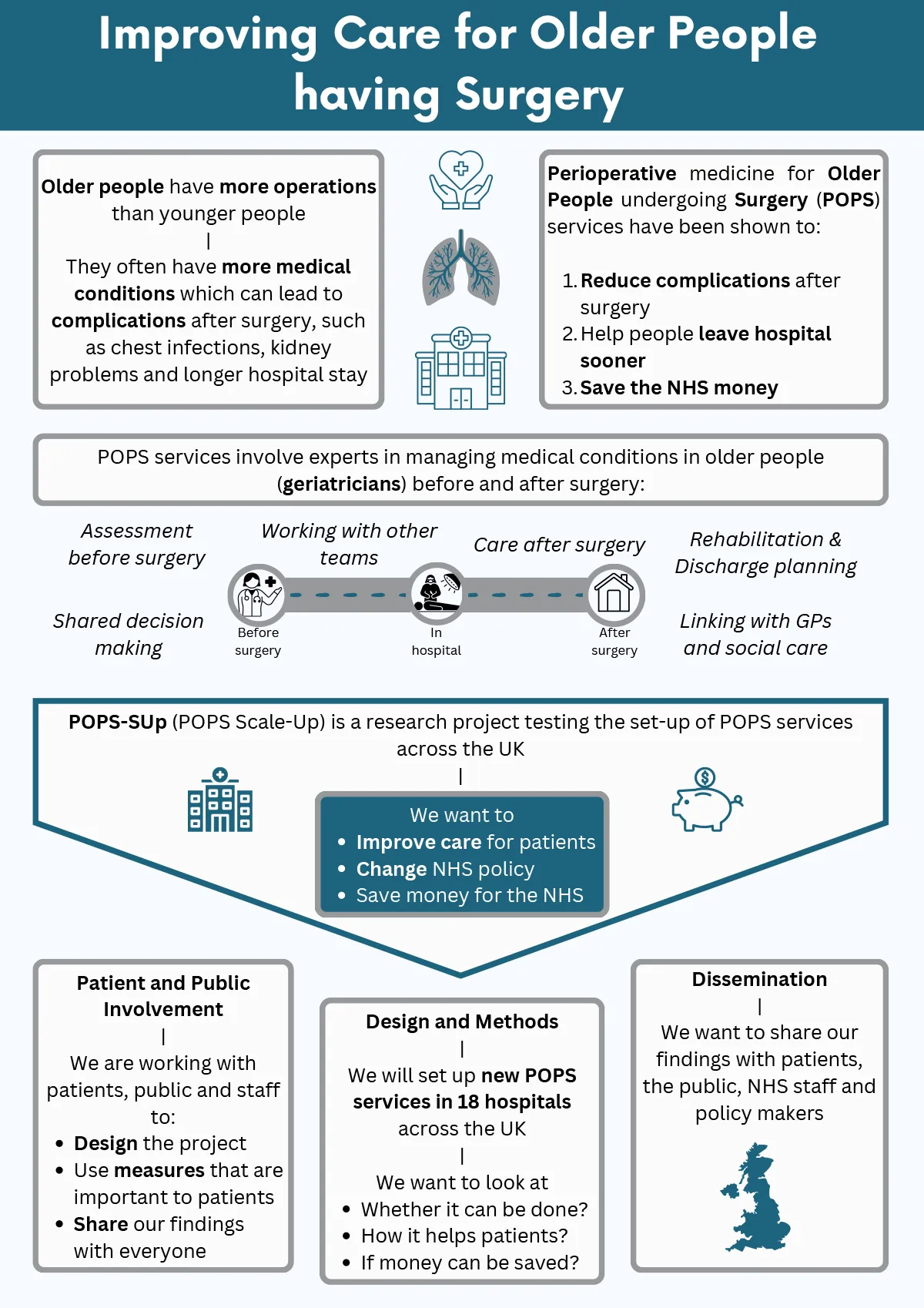
Older people have more operations than younger people and also have more complications after surgery, such as chest infections, kidney problems, slow recovery and longer hospital stay. This is because older people often have other problems like heart disease or poor memory. These problems need treatment from experts called geriatricians. Having geriatricians care for older people who need operations is not standard in the NHS right now. A service called Perioperative medicine for Older People undergoing Surgery (POPS) was set up at one NHS hospital by geriatricians to help older people get better outcomes after operations. POPS was set up together with patients, carers, surgeons, anaesthetists, nurses, therapists and managers. It uses a method of care called Comprehensive Geriatric Assessment. Studies show that using Comprehensive Geriatric Assessment as part of POPS services can reduce complications after surgery, help people leave hospital sooner and save the NHS money. Some NHS hospitals have now set up POPS services, but not all, meaning not all NHS patients get the same quality of care. We know that setting up POPS services can be hard but our work has shown this can be done. Our research will test how POPS services can be set up in more NHS hospitals to improve care for older patients having operations and save money for the NHS.
Patient and Public Involvement and Engagement:
From its conception, the POPS model has actively involved patients and service users in codesign and coproduction to inform research and service design. Through collaboration with PPIE groups, we have continuously gathered feedback to help shape our POPS service and research.
Three stakeholder groups have been established to work with us throughout the study, meeting biannually to allow participants to help shape the study as it progresses:
- PPIE1: Public advisory group of patients and carers with lived experience
- PPIE2: Community of practice/network comprising clinicians delivering NHS POPS services
- PPIE3: Multidisciplinary professional stakeholder group comprising clinicians, professional bodies, charity representatives, decisions makers
Effective PPIE has directly informed the POPS-SUp research question, the use of a hybrid effectiveness-implementation study design, the use of co-primary outcome measures and the dissemination strategy. Furthermore, conversations with patients have provided valuable insights into what matters most to them. It prompted a focus on the inclusion of a shared decision-making approach, ensuring ‘no decision about me, without me’ and a sub-study exploring the impact of mental health issues on perioperative shared decision making. Patients also told us they want to know about delirium and functional recovery with some people eager to hear updates about POPS-SUp in written form.
This PPIE approach to codesign and coproduction of research has been acknowledged by the Royal College of Anaesthetists, Patient Voices Gold Award which we are proud to announce that the GSTT POPS team won earlier this year. We continue to share our learning through PPIE newsletters and recently published a blog with The Patient’s Association: Improving care for older people having surgery through meaningful patient involvement | The Patients Association
Our ongoing commitment to PPIE work continues to guide how POPS is delivered and expanded nationally, ensuring that patient voices remain central to our research and service development.

Internal Steering Committee Members:
|
Name |
Profession |
|
|
Professor Jugdeep Dhesi |
Professor of Geriatric Medicine |
|
|
Dr Emily Henderson |
Consultant geriatrician |
|
|
Professor Ramani Moonsinghe |
Professor of Perioperative Medicine at University College London (UCL) and a Consultant in Anaesthetics and Critical Care Medicine at UCL Hospitals |
|
|
Dr Daniele Bryden |
Consultant in Intensive Care Medicine |
|
|
Professor Janet Peacock |
Emeritus Professor of Medical Statistics |
|
|
Professor Nick Lees |
Consultant General & Colorectal Surgeon |
|
|
Professor Simon Conroy |
Professor of Geriatric Medicine |
|
|
Dr Arabella Scantlebury |
Applied health researcher and social scientist |
|
|
Professor Vasikaran Naganathan |
Consultant Geriatrician |
|
|
Dr Anna Whittle |
Consultant Geriatrician |
|
|
Mr Bob Evans |
Patient Representative |
|
|
Mr Kirit Mistry |
Charity Representative |
|
|
Ms Elizabeth Stokes |
Senior Researcher |
|
|
Dr Bridget Strasser |
Consultant Geriatrician |
Aims
Can CGA-based perioperative medicine services (POPS services) be implemented throughout the NHS, to improve clinical outcomes for older patients undergoing elective and emergency surgery with cost effectiveness?
Methods
We will use our ‘strategy’ to see if we can set up new POPS services in 18 hospitals. We will measure whether we can do this quickly, how well POPS services run, whether POPS services help people to get better more quickly after an operation and whether this saves the NHS money. We will collect information about how long people stay in hospital after an operation, describe complications after surgery and measure patient’s quality of life. We will also talk to patients and staff about their experiences of new POPS services. Our research will use a mix of information from staff, from hospital records and directly from patients and carers. We will look at these data using statistics and by describing common themes. This will tell us if POPS services can be set up across the NHS, whether patients benefit and if money can be saved.
Summary of Findings
The research team have made lots of contacts with patient, public and staff groups such as charities, policy makers and healthcare professional groups. Using these contacts, we will share our findings with patients, the public, NHS staff and policy makers through talks, articles, press releases, social media, videos, websites and meetings to change NHS policy, save money and improve care for patients.
Guy’s and St Thomas’ NHS Foundation Trust are the sole sponsor of the POPS-SUp study.
Impact
Milestones achieved:
- September 2024 Protocol and supporting documents completed
- September 2024 Site identification and enrolment – 9 sites across UK (1 NI, 1 Scotland)
- 4/10/24 CAG approval received
- 7/10/24 HRA favourable opinion received
- November 2024 database development complete
- 11/11/24 Pre-implementation data collection for cohort one commenced
- 13/12/24 ISRCTN registration complete
- 21/05/25 Won RCoA Patient Voices Gold Award for PPIE work
- 05/11/25 Cohort 2 launch event
- Regular PPIE engagement as per protocol
For more information on POPS-SUp
- NHS Futures POPS Network website: Welcome to the POPS Network - POPS Network (Perioperative Care for Older People Undergoing Surgery) - Futures
- POPS-SUp study protocol: Perioperative Medicine for Older People Undergoing Surgery Scale Up (POPS-SUp): study protocol
- ISCTRN Link: ISRCTN - ISRCTN89854824: Perioperative medicine for older people undergoing surgery scale-up
- Linkedin: POPS-SUp Study: Company Page Admin | LinkedIn
- Patient Voices Award: Winners of the PatientsVoices@RCoA Award 2025 | The Royal College of Anaesthetists
- Blog post: Improving care for older people having surgery through meaningful patient involvement | The Patients Association
Principal Investigator
Funding
Funding Body: National Institute for Health Research (NIHR)
Amount: £1,540,771.70
Period: March 2024 - May 2027

