“The pandemic has brought many substantial changes to the lives of children and young people. This is the first time we were able to specifically look at the effects of lockdown measures in an international sample. Lockdowns have impacted self-harm and help-seeking in some young people more than the others, and these differences are also evident in other countries."
Ben Hoi-ching Wong, the study’s first author from King’s IoPPN
29 July 2022
Boys twice as likely to attend hospital for self-harm during strictest lockdowns
Stricter COVID-19 lockdown measures coincided with an increase in serious self-harm triggered by social isolation in children and young people, according to a new study published in BJ Psych Open.
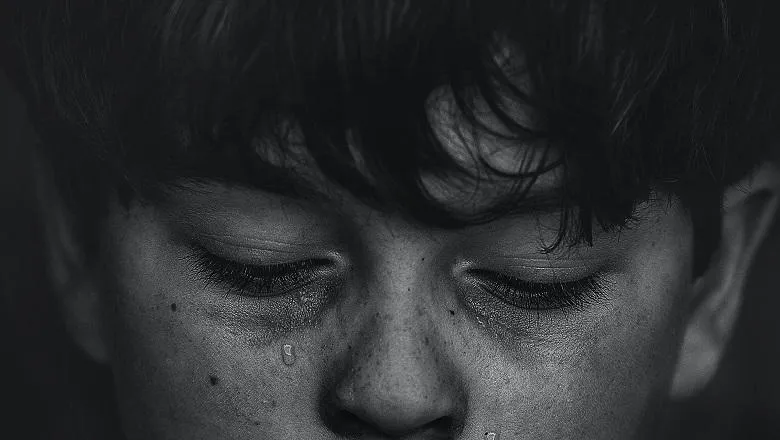
New research from the Institute of Psychiatry, Psychology & Neuroscience (IoPPN) at King’s College London has found that emergency hospital visits for self-harm were twice as likely for boys, and three times as likely for looked-after children, compared to pre-pandemic levels.
The researchers analysed data from 2,073 emergency self-harm hospital visits for children and young people from 10 countries, comparing March to April 2020 with the same period in 2019.
Girls continue to be over-represented in self-harm figures but during the strictest lockdowns, the proportion of boys needing urgent support from emergency services doubled and then tripled for looked-after children.
While self-harm related to social isolation increased during stricter measures, school pressure and rows with friends became less common triggers. However, these closures may have led to greater urges to self-harm, related to increased overthinking and negative coping strategies at home.
Ben Hoi-ching Wong, the study’s first author from King’s IoPPN said, “This research highlights how we need to diversify our approaches to supporting at-risk youths based on their individual needs, and particularly be mindful of addressing their concerns or worries about seeking medical and psychological help.”
Children from more deprived areas became less likely to visit emergency departments, while also having less access to community support networks, suggesting they are at greater risk of “falling through the cracks”.
Similarly, overcrowded living spaces may have increased interpersonal stress within the family. Researchers believe it’s possible that a lack of meaningful social interactions outside of immediate family during lockdown could also play a part due to a shrinking support network.
Recommendations from the report include funding and developing intensive community mental health services and remote-access psychiatry to provide assessment and interventions outside of hospitals, before emergency care is needed.
Dr Elaine Lockhart, Chair of the Child and Adolescent Faculty at the Royal College of Psychiatrists, said, “We know that the majority of young people who self-harm do not seek help from health services. While not all children who self-harm will need psychiatric intervention, we do need to have a full range of mental health support in our communities so that the most unwell can access help quickly. The earlier we offer support, the less likely people are to develop long-term mental health problems.
“It’s important to consider the impact of measures put in place during the pandemic on self-harm so that we can plan mental health services for the future. That’s the only way to ensure all children and young people receive the mental health support they need, when they need it.”
Prior research by the Royal College of Psychiatrists demonstrated how children and young people’s mental health has been severely affected by the pandemic, with more of these patients visiting emergency departments in crisis.
This is confirmed by NHS data that shows self-harm admissions to hospital for 10-24 year olds at their highest levels during the first quarter of 2021-22 following a drastic drop during the first lockdown 2020.
Lockdown stringency and paediatric self-harm presentations during COVID-19 pandemic: retrospective cohort study (DOI:10.1192/bjo.2022.41) (Ben Hoi-ching Wong, Mehrak Vaezinejad, Paul L. Plener, Tauseef Mehdi, Liana Romaniuk, Elizabeth Barrett, Haseena Hussain, Alexandra Lloyd, Jovanka Tolmac, Manish Rao, Sulagna Chakrabarti, Sara Carucci, Omer S. Moghraby, Rachel Elvins, Farah Rozali, Ereni Skouta, Fiona McNicholas, Benjamin Baig, Dejan Stevanovic, Peter Nagy, Chiara Davico, Hassan Mirza, Evren Tufan, Fatima Youssef, Ben Meadowcroft and Dennis Ougrin) was published in BJPsych Open.
For more information, please contact Patrick O'Brien (Senior Media Officer)

