We were astounded to see how effective targeting a specific subset of TAMs was in reducing tumour growth in this model, where ICI therapy had no impact.
Lead author of the study, Professor Toby Lawrence, School of Immunology & Microbial Sciences
02 August 2019
Scientists find potential 'magic bullet' for treating tumours
Researchers have found a therapy to reduce the size of tumours where previous drugs have failed.
Tumours develop from abnormal cells in the body that continue to grow forming lumps. These lumps can be benign, meaning they’re not harmful, or they can become malignant which leads to cancer.
Malignant tumours, become infiltrated by immune cells called macrophages – meaning big eater – these cells usually help the body’s immune defence, but Tumour-Associated Macrophages (TAMs) are manipulated by cancer cells and not only contribute to the growth and spread of tumours in the body, but they also suppress our natural immune defence against them.
Because of TAMs dual action in causing cancers to grow and thrive, researchers from King’s and Institut national de la santé et de la recherche médicale ) have designed a therapy that targets them without suppressing other macrophages. In a study published today in the Journal of Experimental Medicine, researchers have been able to demonstrate how to target the ‘bad’ TAMs whilst not suppressing the body’s own natural defences.
Other recent cancer therapy developments include drugs called immune checkpoint inhibitors (ICI) which have been a revolution in cancer treatment, especially for melanoma patients. However, patients that respond to ICI therapy have severe side effects and more than 70 % of patients don’t respond at all.
In this study, the authors used mouse models of melanoma which are resistant to ICI therapy and were able to target a specifically the bad TAMs which caused massive recruitment of immune cells and significantly reduced the size of tumours.
Lead author of the study, Professor Toby Lawrence believes this could be developed into a drug to specifically kill TAMs and result in a magic bullet which could be directly applied in the clinic.
‘This study not only provides a new strategy for targeting specific TAM subsets in the clinic but also shows why it’s important to target specific TAM subsets and not other macrophages that help anti-tumour immune responses’ – Professor Lawrence.
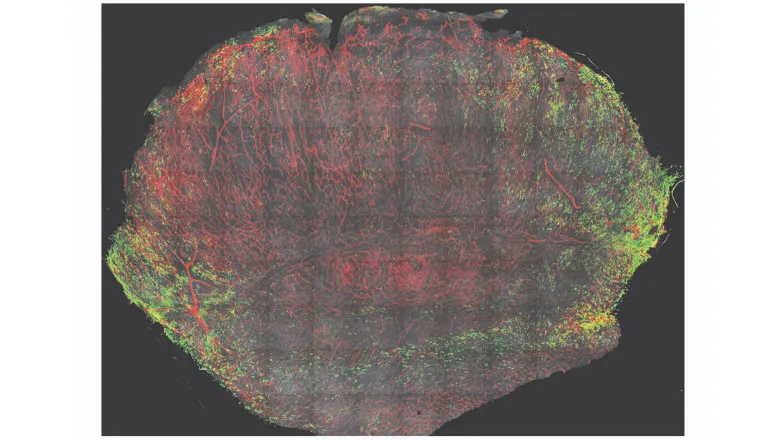
(Image shows a cross-section through a melanoma with CD163+ TAM stained in green, blood vessels stained in red and the nuclei of cells are stained in grey.)
