“This mega-analysis has allowed us to move beyond the limitations of smaller studies. The larger group allows us to account for factors like age, gender, and severity of the disease, and enables us to gain a greater understanding of a life changing illness.”
Professor Mitul Mehta, the study’s lead author from King’s IoPPN
26 January 2022
Structural brain differences found in people with Parkinson's Disease who experience psychosis
New research from the Institute of Psychiatry, Psychology & Neuroscience (IoPPN) at King’s College London has discovered structural brain differences in people with Parkinson’s Disease that do and do not experience hallucinations.
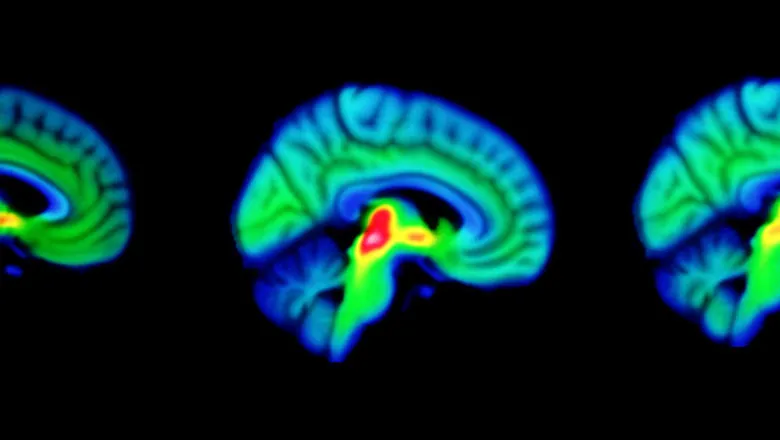
The study, published today in Nature Communications, is the first attempt to gather the structural imaging data from several studies in order to identify the cortical regions and networks that are affected in people experiencing Parkinson’s Psychosis (PDP).
Patients with Parkinson’s Disease can also commonly experience a range of psychiatric symptoms, including visual hallucinations, in addition to the typical motor symptoms. These symptoms can affect up to 70% of Parkinson’s Disease patients in the more advanced stages of the illness, and the development of hallucinations can be a predictor of further cognitive decline.
The researchers conducted a mega-analysis, combining the scans pf patients with Parkinson’s disease, shared by researchers from many different countries. To date, previous studies of visual hallucinations in PD have been based on relatively small samples, and designed differently. This makes it difficult to properly understand the changes that have taken place in someone experiencing psychosis while taking account the variation between patients in other factors such as cognitive decline, or medication dose.
This research collected data from 493 participants, of which 135 experienced symptoms of psychosis. The investigators sought to explore cortical thickness and changes in surface area in the brain, as these separate components reflect different aspects of the neurodegenerative process.
An analysis of the data revealed widespread reductions in cortical thickness in those participants with visual hallucinations. A novel finding was the reduction in thickness and also surface area in the lingual gyrus, a brain structure that is linked to processing vision. The extensive structural changes in the primary visual cortex and the surrounding area could help to account for the wide range of visual deficits found in those people who experience PDP. We also showed extensive involvement of the frontal regions and associated brain structural networks, areas known to be involved with attentional function.
The widespread changes in brain structure were also associated with the pattern of dopamine and serotonin receptors in the brain, neurochemical systems known to be involved in PDP, providing important clues as to which drug systems to test in treatment studies.
Dr Miriam Vignando, the study’s first author from King’s IoPPN said, “This study has been possible thanks to an international collaboration and we have now a very rich dataset. This has allowed us to have a clearer insight in the structural networks involved in PDP and to lay out hypotheses regarding the neurotransmitters involved. To further understand and clarify this, we are looking forward to investigating some of our interesting results looking into greater detail at subcortical structures and adding other neurotransmitters to the analyses.”
This study was possible thanks to funding from the Medical Research Council and The NIHR Maudsley Biomedical Research Centre.
Mapping brain structural differences and neuroreceptor correlates in Parkinson’s disease visual hallucinations (DOI 10.1038/s41467-022-28087-0) (Miriam Vignando, Dominic ffytche, Simon Lewis, Phil Hyu Lee, Seok Jong Chung, Rimona S. Weil, Michele T. Hu, Clare E. Mackay, Ludovica Griffanti, Delphine Pins, Kathy Dujardin, Renaud Jardri, John-Paul Taylor, Michael Firbank, Grainne McAlonan, Henry K. F. Mak, Shu Leong Ho & Mitul A. Mehta) was published in Nature Communications.
For more information, please contact Patrick O'Brien (Senior Media Officer)


