These findings highlight the importance of looking beyond standard genetic testing. They lay the groundwork for more accurate risk assessment and could help guide the development of new immune-based stratification and treatments for MDS. Instead of focusing solely on gene mutations, it’s crucial to also consider how the disease disrupts the immune system and other key biological processes and include these factors in the current risk stratification.”
Co-lead author Dr Shahram Kordasti, Reader and Group Leader in Applied Cancer Immunopathology
11 June 2025
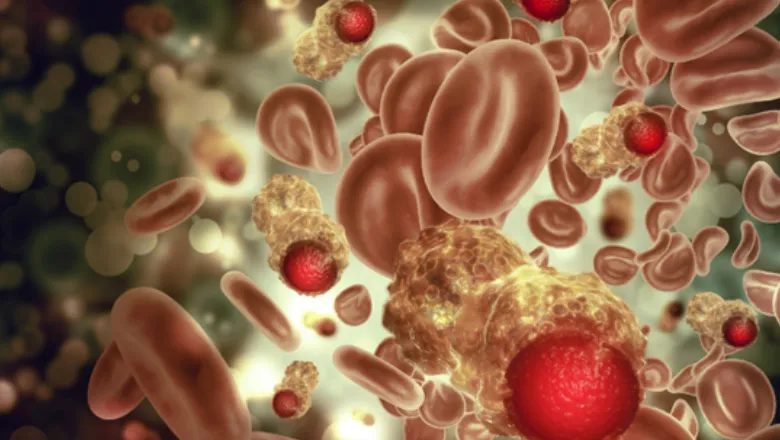
Study reveals immune drivers of aggressive blood cancer
Researchers have uncovered why certain myelodysplastic syndromes (MDS) patients experience more aggressive disease and poor treatment response, despite having no detectable adverse genetic mutations.
The study, published in the Journal of Clinical Oncology, focuses on the role of p53, a protein that normally helps control cell growth and repair. Although mutations in the TP53 gene are known to worsen outcomes in MDS, this study found that the p53 protein can stop working properly even when the gene appears normal.
MDS is a group of blood cancers that affect how the bone marrow makes healthy blood cells. Some forms progress slowly, while others can rapidly turn into acute myeloid leukaemia (AML). Accurately identifying patients who are at higher risk is vital for guiding treatment decisions.
Understanding p53 dysfunction
Led by Drs Shahram Kordasti, King’s, Francesca Ficara, IRCCS Humanitas Hospital, Italy and Matteo Giovanni Della Porta, Humanitas Hospital, Italy, the researchers analysed data from more than 6,000 people with MDS using techniques such as IHC, RNA sequencing, immune cell profiling, and single-cell analysis. They identified a group of patients with normal TP53 genes but high levels of abnormal p53 protein in their bone marrow, finding that these patients had worse outcomes than others.
The dysfunction was linked to disruptions in key cell signalling pathways and an increase in copies of the MDM2 gene, which is known to block p53’s activity. As a result, the protective role of p53 was lost, even without any genetic mutation.
Immune system impact
Crucially, the study found that p53 dysfunction was also associated with a suppressed immune environment in the bone marrow. Key immune cells, such as T cells and natural killer (NK) cells, were exhausted or less active, and a specific type of T cells, known as regulatory T cells (Tregs) were expanded and cancer cells were better at hiding from immune attack. This may partly explain why these patients respond poorly to current treatments.
The results suggest that combining genetic, functional testing and immune signatures, could help clinicians identify high-risk patients more effectively. The study also supports a broader approach to classifying MDS and opens the door to more personalised, immune-targeted treatments in the future.

