Body Worn Cameras on Inpatient Mental Health Wards
Plain English Summary
When mental health service users are admitted to hospital, often at a time of great distress, inpatient wards are regarded as safe places that should facilitate assessment and treatment in a calm, therapeutic environment.
However, sometimes inpatient wards can have worrying levels of violence and aggression. This can make the ward feel unsafe for both service users and staff, cause injuries and complaints, and ultimately slow down a service user’s recovery.
Therefore, reducing violence and aggression is a main priority for all mental health inpatient wards. For many years, staff have tried different approaches to address this problem, including strategies to improve the therapeutic environment on the wards, such as the Safewards model (www.safewards.net) as well as better monitoring through the introduction of new technologies like CCTV.
Some inpatient wards have now also started to use Body Worn Cameras (BWCs) that staff can attach to their clothing and then activate to record both video and sound of interactions and incidents that happen on the ward. This kind of technology is already routinely used by the police and other public services, and it is now quickly being rolled out in healthcare settings as well.
However, BWCs are still very new to many mental health services. There is only limited research about their use on inpatient wards, and most studies have not considered the perspectives of services users so far.
Our study is specifically designed to address this gap. We are planning to carry out in-depth interviews to explore the views and experiences of mental health service users and staff regarding the use of BWCs in acute inpatient mental health settings. We hope that the information we collect is eventually going to help inform how such technology can be used ethically and safely, or whether it should be used at all.
We are committed to involving people with relevant lived experience throughout the study from start to finish. Therefore, we have been working closely with an independent service user collaborator who is part of the research team and have also employed two Lived Experience Research Assistants to work on the study. Finally, we are involving service user representatives from diverse backgrounds on a Lived Experience Advisory Panel (LEAP), who will act as critical friends to advise on all aspects of the study’s development and coordination.
Background
As part of the violence reduction strategy reported by the Government in 2018, the health secretary Matt Hancock announced he was pursuing the use of Body Worn Cameras by NHS staff to deter violence. Body worn cameras (BWC) are mobile audio and video capture devices that can be secured to various parts of the body using different types of attachment, allowing the wearer to record what they see and hear.
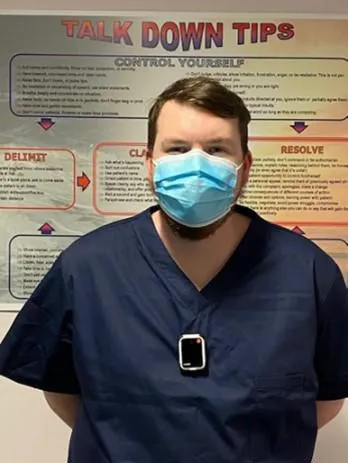
© Photo provided courtesy of Northamptonshire Healthcare NHS Trust
Anecdotal evidence suggests reductions in violence and complaints as a result of the use of BWCs across the NHS in settings such as accident and emergency departments and within forensic mental health settings (Millard, 2015; Tully, Larkin & Fahy, 2015). However, published evaluations to support these claims are limited due to the lack of comparison across contexts, limited quality of studies and the absence of longitudinal data. There are tentatively promising results regarding the application of BWCs in inpatient mental health settings that suggest potential use in helping to de-escalate aggressive encounters and to provide transparency in challenging nurse-patient interactions and use of restraints (e.g., Hardy, Bennett, Rosen, White & Palmer-Hill, 2017). However, there is a need to further understand the acceptability and usability of such technology within mental health settings in which coercion and capacity remain prominent issues to consider and where a growing proportion of patients are detained under the Mental Health Act (DHSC 2018, p.20). Some of these issues were debated at the Royal College of Nursing (RCN) congress in 2018, raising key concerns regarding the impact of such technology on patient-nurse relationships, confidentiality and ethical issues, and concerns surrounding the capacity and consent of patients to being filmed.
The use of this technology has been increasingly employed within law enforcement and police services as the BWC are intended to provide transparency and internal accountability particularly within use-of-force incidents and in the event of citizen complaints (Gaub, Choate, Todak, Katz, & White, 2016; Miller & Toliver, 2014). An early study in law enforcement suggests that the use of BWCs has the potential to reduce the likelihood of force being used in this context (Ariel, Farrar & Sutherland, 2015). As a result, the use of BWCs has been explored in wider contexts in which transparency around force may be required, including the recent introduction of ‘Seni’s Law’ that requires police attending mental health settings to wear body cameras as part of the Mental Health Units (use of force) Act (2018). Such technology may provide opportunities to identify integral problems within the organisation, improve evidence documentation, reduce use-of-force incidents, improve police-community relations, and provide training opportunities (Cubitt, Lesic, Myers & Corry,2017). However, although this technology is increasingly used and accepted within police services across the UK and USA, it is unclear whether and how the use of BWC changes behaviours and there is limited evidence to determine whether the perceived benefits of these devices justify their costs or potentially adverse impacts (e.g., Lum et al. 2020).
It is important that if this technology is to be implemented within mental health care settings that research is conducted to explore the views, experiences and any concerns of service users and staff. There has been little investigation of staff views concerning these and other issues related to the deployment and use of BWCs, and even less attention given to the views of mental health service users. Debates following the publication of an article on BWCs in mental health settings (Mulholland, 2019) and discussions on web-based forums for mental health service managers and senior clinicians has seen strong views and concerns expressed by service users (and some mental health nurses) on social media platforms and in mental health publications (Rowan Olive, 2019). With the growing implementation of such technologies and the policy drive increasing the use of BWCs in healthcare settings, it is surprising that there is such a dearth of research considering the patient voice within the debate surrounding the topic. Therefore, the current study will explore the experiences and perspectives of service users, mental health staff and senior management to understand the motivations, concerns, barriers, impact, and unintended/adverse consequences of such technological use. This study will empirical data, new theoretical knowledge, and greater understanding of this complex issue to inform policies and practice in this area.
The Qualitative Study
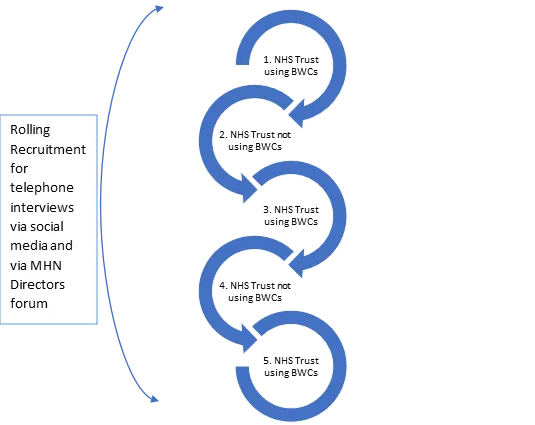
To help understand the perceptions and experiences of service users and staff on wards regarding the use, or possible use of BWCs, we are undertaking an exploratory study in which we will interview a wide range of service users and staff working across a range of mental health trusts, and via social media.
During these interviews, we will explore the experiences and perspectives towards the use of BWC technology in acute mental health wards amongst staff managing or working on wards as well as those with experience of inpatient admission on acute wards. We will talk to people across several wards where BWC technology is currently being used as well as wards where this technology has not been used, yet. This will allow us to explore and compare the experiences of introducing, employing and being subject to the use of this technology, as well as the perceptions, motivations, expectations and/or concerns of those where it may or may not be implemented in the future. This is so we can reflect the wide range of people with experience of being a patient on inpatient mental health wards to understand the impact of these cameras as fully as possible.
Lived Experience Advisory Panel
We were overwhelmed by responses to our call for applicants to form a Lived Experience Advisory Panel for this project. We have now recruited a diverse panel of 8 people with inpatient mental health experience to support and advise our study, helping our research team to understand their work from a service user point of view.
We hope to offer more opportunities for involvement in the future. If you want to keep up to date with the progress of the study and activities of the LEAP, please click here to sign up to our mailing list for periodic email updates.
Awards
The Body Worn Cameras on Inpatient Mental Health Wards study is funded by the Maudsley Charity and the Florence Nightingale Faculty of Nursing, Midwifery and Palliative Care Research Challenge Fund 2019

