We need work out the best way to monitor response to treatment for patients with brain tumours but this is a challenging task because there are many different types of brain tumours and each patient responds differently to treatment.
Dr Tom Booth, Senior Lecturer in Neuroimaging
09 February 2021
Changes should be made to routine scans for brain tumours, say researchers
A new Position Statement from UK stakeholders highlights evidence gaps for routine follow up brain tumor imaging, but paves the way for evidence-based imaging
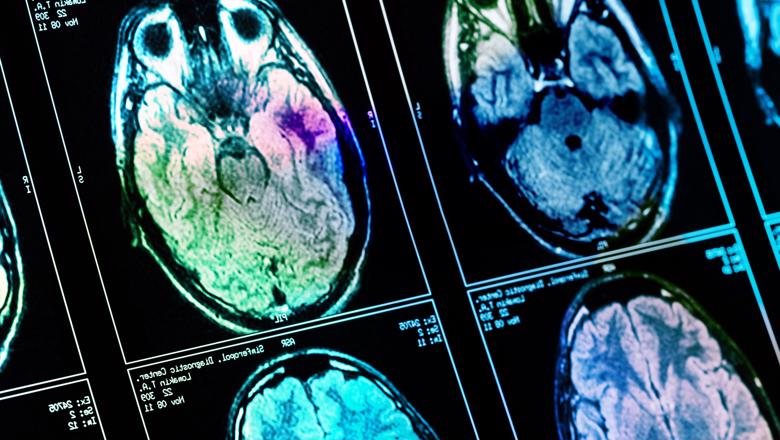
Researchers from the School of Biomedical Engineering & Imaging Sciences are part of a large group of UK experts having released a position statement highlighting the evidence behind current scanning routines as weak, claiming after patient treatment, medical staff use routine brain scans to monitor progress in brain tumor patients, but the best frequency of such scans is unclear. The experts posit solutions for researchers to better gather evidence to improve scanning routines that are more effective and do not interfere with patient quality of life.
Published today in Frontiers in Oncology, the position statement suggests there is limited evidence to support interval imaging, the practice of routinely imaging brain tumour patients to assess their tumour treatment response. The researchers say the status quo is no more than considered opinion but providing realistic and nuanced pathways to obtain the necessary evidence.
Lead researcher, Dr Tom Booth, senior lecturer in neuroimaging at the School of Biomedical Engineering & Imaging Sciences, said researchers including charity representatives, neuro-oncologists, neurosurgeons, neurologists, neuro-psychologists, trialists, health economists, data scientists and the imaging industry met in 2019 in London and found patients and clinicians have different perspectives on the use of interval imaging, as a brain scan only gives a snapshot view of the brain tumour at a specified time.
Dr Booth said brain tumours are disproportionately devastating. Malignant glioma for instance, is uncommon, 5 per 100,000 people but causes more adult working days of life lost than other cancers.
Brain tumours also have complex treatment regimens and can involve surgery, radiotherapy and chemotherapy. Together the treatment complexity and relative rarity mean that solutions beyond traditional "randomised controlled trials" alone are required to obtain the necessary evidence.
“Better research is needed including using machine learning and we offer a range of incremental research solutions,” Dr Booth said.
The researchers say economic and statistical analyses, surveys to measure patient attitudes and quality of life while undergoing interval imaging, and even machine-learning methods are needed to obtain more accurate predictions about the value of interval imaging from large datasets.
Medical staff use brain scans at predetermined times to assess if a brain tumour patient is responding to treatment, but scanning can range from every few weeks to months.
However, while not scanning someone enough could mean that doctors miss the signs that a patient requires further treatment, conversely, scanning someone excessively is inconvenient and impractical for patients and medical staff alike, and can cause patient anxiety, especially if the results of the scan are unclear.
Scanning patients is also expensive, and with limited budgets, healthcare facilities need to use their resources as cost-effectively as possible.
Most interval imaging aims to find increases in tumor size, but tumors grow differently in different patients, which sometimes makes it difficult to draw concrete conclusions from interval imaging results.
Future research is key to assessing and maximizing the potential of interval imaging.




