Prenatal ThERapy for SIckle CelL disEaSe (PERICLES)
This research project focuses on developing tools and methodologies for Sickle Cell Disease (SCD) research. We aim to understand how prenatal therapy can be used to treat SCD by developing gene-editing approaches in human and mouse fetal haematopoietic stem cells (HSCs) and delivery methods in a mouse model of SCD. In addition, we aim to generate new knowledge on the ethical considerations and the stakeholders' views on the acceptability of this therapy.
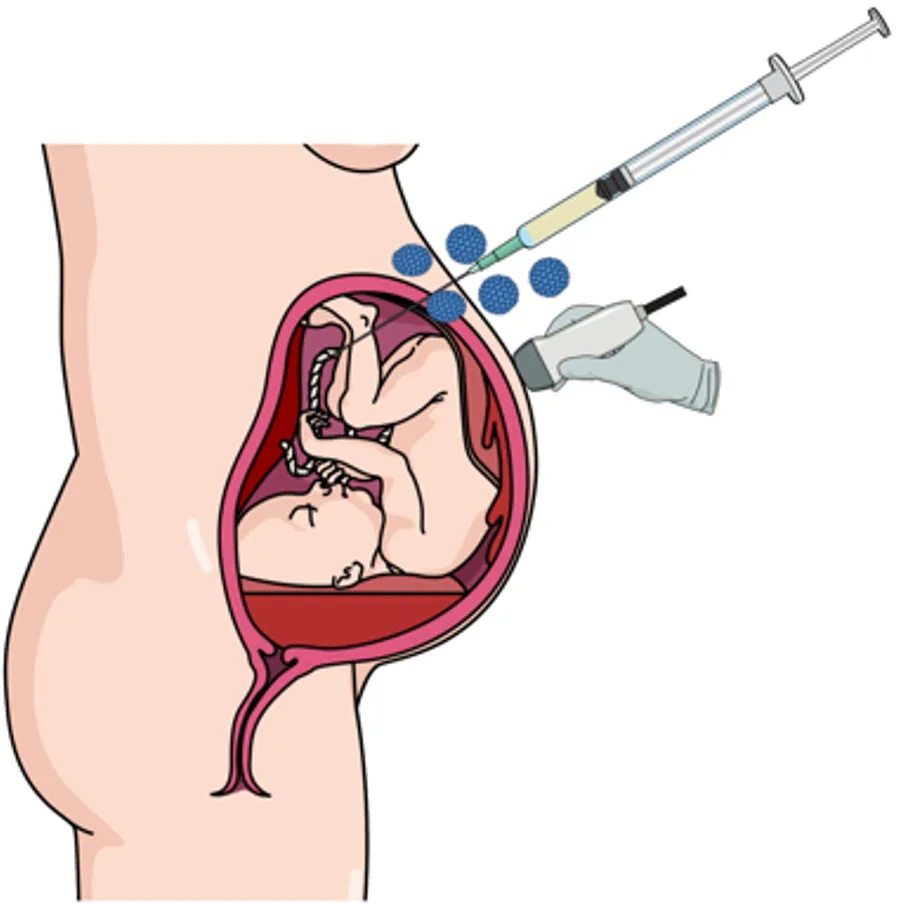
Sickle Cell Disease (SCD) is a severe, progressively debilitating, and life-threatening genetic disease, which results in frequent vaso-occlusive episodes and anaemia, causing chronic organ damage, infections and strokes in children and adults1. In Africa, it accounts for 9-15% of all deaths of children, and it is expected to rise to 400000 births per year in 20501. SCD results in poor quality of life and, in many cases, a significantly shortened lifespan. Most available treatments only manage symptoms1 and are estimated at $460000 over the patient's lifetime2,3. SCD associated admissions cost the NHS £18 million in 2010-20114. There are around 4000 patients under King's Health Partners, about a third of all SCD patients in the UK. A cell or gene therapy for SCD is likely to be cost-effective in adult SCD patients5 and will be even more cost-effective if a SCD fetus is born disease-free. The development of non-invasive prenatal diagnosis using circulating fetal DNA from the mother's blood allows the early detection of congenital fetal diseases from ten weeks of gestation 6,7. Currently, the two main options are 1) termination of pregnancy or 2) careful monitoring and delivery followed by post-natal treatment where appropriate. This proposal addresses a potential third option; in utero treatment of SCD by delivering the corrected version of a cell and or gene before birth.
This project has been granted full approval by the BDM Research Ethics Panel: LRS/DP-22/23-27087: Stakeholder views and attitudes towards Prenatal Therapy for Sickle Cell Disease (SCD)
Aims
To generate new knowledge about stakeholders' views on prenatal therapy8 for SCD, to understand perceived benefits or concerns, identify ethical issues and establish protocols for support and counselling.
Methods
- Up to 30 one-to-one interviews with stakeholders, including women of childbearing age who either have SCD or are carriers of SCD, healthcare professionals who work with patients with SCD and patient advocates from the Sickle Cell Society.
Under the guidance of Dr Celine Lewis, Senior social scientist at the University College London, we will perform a qualitative exploration of experience and perceptions with template analysis using an Acceptability Framework to code, sort, and interpret data. This study will generate insights and will allow us to understand the acceptability around clinicians delivery of stem cell or gene-editing therapies in utero as an alternative option to terminating the pregnancy or waiting for postnatal management8–11. For example, in a similar study co-authored by Dr Celine Lewis (UCL), the senior social scientist and advisor in this fellowship, they found that most people held positive views towards using in utero stem cell therapy to treat Osteogenesis imperfecta (OI)8.
Impact
A positive opinion from the stakeholders is critically important in the development and funding of this project. If there is no treatment, clinicians are faced with offering termination of pregnancy or delivery of an affected baby. This would have a huge impact, especially in African countries where termination of pregnancy may not be available, medications and blood transfusions are prohibitively expensive, and SCD is most prevalent. Clinicians working with patients with sickle cell disease might also benefit from this therapy and might see the patients for pre-pregnancy counselling. The potential of this treatment can be part of pre-pregnancy counselling alongside the option of preimplantation genetic diagnosis. In addition, Clinical Geneticists might also include this therapy in their prenatal counselling and use any co-inherited mutations to predict the severity of the disease.