First network analysis of patient flow in two UK hospitals published
Researchers at the Institute of Psychiatry, Psychology & Neuroscience (IoPPN) at King’s College London and King’s College Hospital NHS Foundation Trust, have used network science to analyse patient flow through a hospital for the first time in a UK health system.
The results of their data-driven network analysis were published in October in PLOS ONE.
The report authors were Dr Daniel Bean and Professor Richard Dobson, Department of Biostatistics and Health Informatics, IoPPN, King’s College London, and Clive Stringer, Dr James Teo and Neeraj Beeknoo, King’s College Hospital.
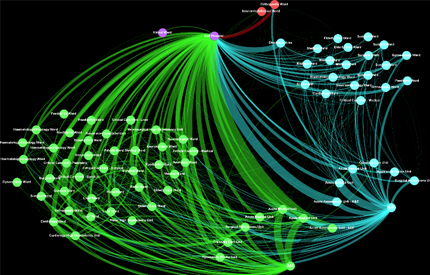 A Patient flow network for a 6-month period. Each circle (“node”) represents a single hospital ward. The wards are connected by lines (“edges”) when patients are transferred between them. The thickness of each edge represents the number of patients who took that path through the hospital network. These networks are the basis for the recent patient flow analysis.
A Patient flow network for a 6-month period. Each circle (“node”) represents a single hospital ward. The wards are connected by lines (“edges”) when patients are transferred between them. The thickness of each edge represents the number of patients who took that path through the hospital network. These networks are the basis for the recent patient flow analysis.
The researchers looked at 18 months’ worth of data from the patient administration system and the electronic patient record at King’s College Hospital, Denmark Hill, and the Princess Royal University Hospital, both of which belong to the King’s College Hospital NHS Foundation Trust ICT network.
The patient transfer data contained more than 78,000 hospital admissions over 578 days.
Their analysis first confirmed prior data showing A&E attendance rate is poorly correlated with hospital performance statistics which suggests there must be other factors affecting performance, beyond simply the volume of patients.
Using graph theory researchers modelled the flow of patients through the two hospitals as a directed flow network (pictured above). Green nodes and edges are in King’s College Hospital, turquoise ones are in the Princess Royal University Hospital and the red ones are outside the King’s College Hospital NHS Foundation Trust network
The key finding of this study was the identification of patterns of patient flow that were associated with extremes of A&E performance against the UK 4-hour waiting time target.
Dr Daniel Bean from the IoPPN at King’s College London, comments, ‘We’ve shown there’s a lot of potential in using graph theory to model patient flow. We can prioritise parts of a hospital that are important for day-to-day functioning and also find specific pathways that changed either when A&E was really struggling, or when it was doing really well. I think it’s important to look at what’s happing in both situations and try to learn from them going forward.’
In both hospitals, greater use of clinical decision units (CDU) was associated with very high A&E performance. The CDUs are used for observation and triage of patients from A&E who may require admission to hospital but no decision has been made yet. Dedicated observation units may help improve flow by reducing unnecessary admissions or misallocation of patients to the wrong specialties.
Dr Daniel Bean continues, ‘We looked at patient flow between wards within two hospitals, but all the components of the entire healthcare system are connected by the people using them. Health data is increasingly digital which means that in the future we could combine data from hospitals, GPs and social care and then use that Big Data to model healthcare on a very large scale.’
The research was funded by the National Institute for Health Research (NIHR) Biomedical Research Centre at South London and Maudsley NHS Foundation Trust and King’s College London.
Notes to Editors
Bean DM, Stringer C, Beeknoo N, Teo J, Dobson RJB (2017) Network analysis of patient flow in two UK acute care hospitals identifies key sub-networks for A&E performance. PLoS ONE 12
(10): e0185912.