Researchers uncover the source of diabetic pain
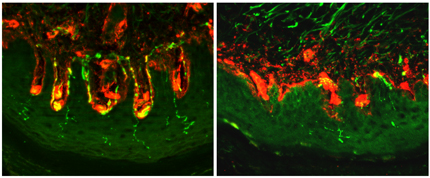
Image (left) shows nerve fibres (green) in a normal mouse, while the loss of nerve fibres in a diabetic mouse is clearly visible in the image on the right. Human diabetic patients show a similar loss of nerve fibres and the activity of HCN2 in these fibres is associated with the development of pain.
A new King’s College London study reveals the molecular basis of chronic nerve pain in diabetes. The findings in mice, published today in Science Translational Medicine, could one day lead to treatments which target the source of the pain.
Around one in four people with diabetes develop a chronic pain condition induced by nerve damage, called painful diabetic neuropathy (PDN), due to high blood sugar. Symptoms include prickling and tingling sensations as well as sharp, shooting pains and extreme sensitivity to touch in the feet and hands, which can spread upward into the legs and arms. The pain can significantly impair mobility, which in turn exacerbates obesity and worsens type 2 diabetes in a self-perpetuating cycle.
Diabetic pain is very difficult to treat and the molecular causes are poorly understood. This new King’s College London study provides the first evidence that a single protein molecule - HCN2 - can by itself be responsible for a complex sensation such as diabetic pain.
The researchers used mouse models of diabetes to show that over-activity of HCN2, which initiates electrical signals in pain-sensitive nerve fibres, results in a sensation of pain. They also found that blocking the activity of HCN2, or removing it completely from pain-sensitive nerve fibres, stopped the sensation of pain entirely.
Professor Peter McNaughton, senior author of the study, from the Wolfson Centre for Age-Related Diseases at King’s College London, said: ‘The inexorable rise of obesity worldwide, in both rich and poorer countries, has brought a related increase in type 2 diabetes. As many as one in four diabetics suffer from nerve pain, yet there are currently no effective treatments and people therefore typically must resign themselves to a life of continuous suffering.
‘Our study reveals the molecular mechanism driving diabetic pain in mice, which we hope will inform future treatments in people with diabetes.’
Dr Christoforos Tsantoulas, first author of the study, also from the Wolfson Centre for Age-Related Diseases at King’s College London, said: ‘At present we do not have selective drugs which can suppress the activity of HCN2 without affecting other bodily functions, such as the regulation of heart rate. This research provides a stimulus for the development of targeted pain drugs that can block HCN2 without affecting the activity of other molecules.’
The main funder of this study was the Medical Research Council (MRC).
Notes to editors
For further media information please contact Jack Stonebridge, Senior Press Officer, Institute of Psychiatry, Psychology & Neuroscience, King’s College London on jack.stonebridge@kcl.ac.uk or 020 7848 5377.
Tsantoulas, C et al. (2017) Hyperpolarization-activated cyclic nucleotide-gated 2 (HCN2) ion channels drive pain in mouse models of diabetic neuropathy. Sci. Transl. Med.