Gene-edited mice may hold key to motor neurone disease
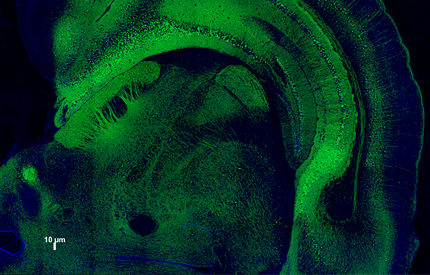
(image: King's College London and the Babraham Institute)
New research has provided strong evidence for a biological mechanism that underpins motor neurone disease (MND). Researchers from King’s College London, the Babraham Institute and the University of Cambridge have created a new mouse model of MND which mirrors the human condition more closely than ever before and reveals a pool of over 450 genes associated with resistance to the neurodegenerative disease.
MND, also referred to as amyotrophic lateral sclerosis (ALS), kills around 1200 people each year in the UK. The disease causes the body’s muscles to fail, impacting walking, speech, eating and eventually breathing. The cause of MND is poorly understood and effective treatments are urgently needed.
In a study published in Nature Neuroscience, the researchers used the gene-editing tool CRISPR to precisely mutate the gene that produces the protein TDP-43. Previous research from King’s College London’s Institute of Psychiatry, Psychology & Neuroscience (IoPPN) found mutations in the TDP-43 gene in some patients with MND. Build-up of TDP-43 occurs across almost all MND patients suggesting a central role for the protein, but how TDP-43 actually causes disease has remained unclear.
‘Our most exciting finding was that there was a disturbance in the way TDP-43 regulates itself in the mutant mice,’ says senior author Dr Jemeen Sreedharan from the IoPPN and the Babraham Institute. ‘The disturbance of this one process causes a whole range of changes across the genome and may be the underlying mechanism responsible for MND.’
Previous mouse models have focused on boosting TDP-43 levels to simulate the build-up seen in humans with MND. However, TDP-43 normally reduces its own production when there is too much and it was this self-reducing process that was disrupted in the new mouse model. As a result of the disruption not only was there a build-up of TDP-43 but other genetic changes were seen including changes to the gene that makes tau, an important protein linked to Alzheimer’s disease and frontotemporal dementia.
MND affects people differently and some patients with genetic mutations don’t get the disease. Even with identical twins one twin might get disease and the other might not. The researchers found the same thing in their mice: some appeared to be more resistant to disease. By comparing gene expression between mice that behaved normally compared to those that were sick the researchers identified genes that could help prevent development of MND.
‘Our study has found over 450 genes that are linked with improved behaviour,’ says Dr Sreedharan. ‘This list includes 30 genes associated with cells in the myelin sheaths that protect nerve cells in the brain. Our results suggest that by increasing the function of these cells we may be able to stave off neurodegenerative effects of TDP-43.’
The researchers are now studying cells from patients with MND who have TDP-43 mutations to better understand the delicate balancing mechanisms controlling TDP-43 levels. They hope that by understanding this process it may be possible to stop the chain reaction that occurs when TDP-43 levels are disturbed, opening the door to a treatment for MND.
Paper reference
‘TDP-43 gains function due to perturbed autoregulation in a Tardbp knock-in mouse model of ALS-FTD’, White et al, Nature Neuroscience, DOI: 10.1038/s41593-018-0113-5
Contact
For further media information please contact Robin Bisson, Senior Press Officer, Institute of Psychiatry, Psychology & Neuroscience, King’s College London, robin.bisson@kcl.ac.uk / +44 20 7848 5377 / +44 7718 697176.