Clinical cardiology
Russell Claude Brock (1903-1980), who graduated from Guy’s Hospital Medical School in 1928, was one of heart surgery’s pioneers. Indeed, his interest in heart surgery came at time when most established medical opinion believed that heart surgery should not be contemplated. Brock held consultant appointments at Guy’s and Brompton Hospitals from 1936 to 1968 during which time his achievements gave him a widespread reputation.
During World War II Brock was thoracic surgeon and regional adviser in thoracic surgery to the Emergency Medical Service in the Guy’s region. Following the war, thoracic surgery techniques and particularly open heartsurgery developed rapidly.
Brock played a major part in pioneering the surgical relief of mitral stenosis and other valvular lesions of the heart. He introduced the technique to correct pulmonary artery stenosis and right ventricular outflow tract obstruction in the beating heart. Brock’s clinical experience demonstrated that even a severely underdeveloped pulmonary outflow tract could be restored to full growth by a successful direct operation.

Guy’s and blue babies
Guy’s surgeon Donald Ross performed the first total correction of Fallot’s tetralogy (or so called ‘blue baby syndrome’) on a patient under one year of age in 1961. The baby was the youngest reported survivor of total correction of Fallot’s by open heart surgery. Now 45, he is also the longest survivor in the world. Ross went on to work at the National Heart Hospital where he performed the UK’s first heart transplant in 1968. The very first ‘blue baby’ operation at Guy’s was in 1947 by world-famous American heart surgeon Alfred Blalock (front centre; visited Guy’s in 1947 and saved the lives of eight British children with the ‘blue baby’ heart condition.) of Johns Hopkins Medical School. Blalock was visiting the medical school as part of a newly established exchange programme between Johns Hopkins and Guy’s Medical School. This exchange programme continues to this day.
Most open heart operations are conducted on a paralyzed heart – cardioplegia – and on coronary bypass. Cardioplegia obviously needs to be safe and reversible. One of the most notable achievements in cardiac surgery was the development of efficient cardioplegic solutions by the biochemist David Hearse at St Thomas’ in the 1970s and 1980s. Operating on the main blood vessels of the body – vascular surgery – was another major advance in treating disease of conditions due to partial or complete obstruction of arteries or, less commonly, veins. Sir Norman Browse (b 1931), Professor of Surgery at St Thomas’, and President of the Royal College of Surgeons from 1992-1995, contributed to this field by popularizing carotid endarterectomy to relieve or prevent cerebral ischaemia.
Abnormal rhythms of the heart – cardiac arrhythmias – are a common cause of illness and death, and although more common in the elderly can also affect children and young adults. The now routine use of cardiac pacemakers currently used for 25,000 patients per annum has transformed the prognosis for many of these patients. Edgar Sowton (1930-1994) was an unusual medical student, gaining simultaneous degrees in physics and medicine at Cambridge. He turned this basic knowledge to good effect in his internationally recognized achievement on the development of cardiac pacemakers and the study of cardiac arrhythmias. He started this work at the Institute of Cardiology, London, and continued it on his appointment to Guy’s.
Stimulating the heart
Edgar Sowton’s career at the Karolinska in Stockholm, the National Heart Hospital in London and then at Guy’s, was devoted to the new clinical science of electrical stimulation of the heart. In the 1960s he became one of the world’s pioneers in the development of pacemakers. He was also one of the first people in the UK to perform coronary angioplasty. The biannual King’s Edgar Sowton Memorial Lecture was established in his memory after his death in 1994.
Biopsy of the heart posed a very difficult problem because of its relative inaccessibility and the risk of bleeding until the development by Peter Richardson at King’s College Hospital of endomyocardial biopsy in the 1970s. This technique is now used world-wide, with the instrument still termed the ‘King’s bioptome’.
Paediatric cardiology has been a strength at Guy’s since its inception. Under the guidance of Michael Tynan (b 1934) the Guy’s team grew an international reputation for its management of congenital heart disease. Surgical and invasive imaging techniques for correcting congenital abnormalities as well as innovations in diagnostic ultrasound all had an important impact on the specialty. These techniques were also developed for se in utero, contributing to the rise of the new discipline of fetal cardiology.
Current research follows in the traditions of the pioneering cardiac and vascular physiology dating back to the days of Starling as well as applied work on the diagnosis and treatment of coronary artery disease and heart failure.
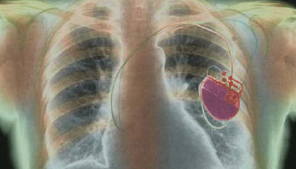
A cardiac pacemaker in place. Pacemakers have transformed the lives of thousands of patients with cardiac arrhythmis.